Periodontal disease, commonly known as gum disease, encompasses a range of inflammatory conditions affecting the tissues surrounding the teeth. This complex disease is primarily caused by bacterial infections that can lead to the destruction of the supporting structures of the teeth, including the gums, periodontal ligament, and alveolar bone. Modern theories of periodontal disease have evolved significantly, integrating insights from microbiology, immunology, and genetics to better understand the etiology, progression, and treatment of this pervasive condition.
What Is The Current Theory of Periodontal Disease?
The Role of Dental Plaque
Dental plaque, a biofilm that forms on the surfaces of teeth, is central to the development of periodontal disease. Plaque harbors a diverse community of microorganisms, including bacteria, viruses, and fungi, which interact with each other and the host tissues. Among the myriad of bacteria present, certain pathogenic species are particularly implicated in the initiation and progression of periodontal disease.
see also: Can My Teeth Be Saved If I Have Periodontal Disease
Key Periodontal Pathogens
Three key bacterial species are often highlighted in the context of periodontal disease: Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola. Collectively known as the “red complex,” these bacteria exhibit several virulence factors that enable them to evade the host’s immune response, adhere to and invade epithelial cells, and cause tissue destruction. The colonization and proliferation of these pathogens in the subgingival biofilm are crucial events in the pathogenesis of periodontal disease.
The Host Immune Response
Inflammation and Tissue Destruction
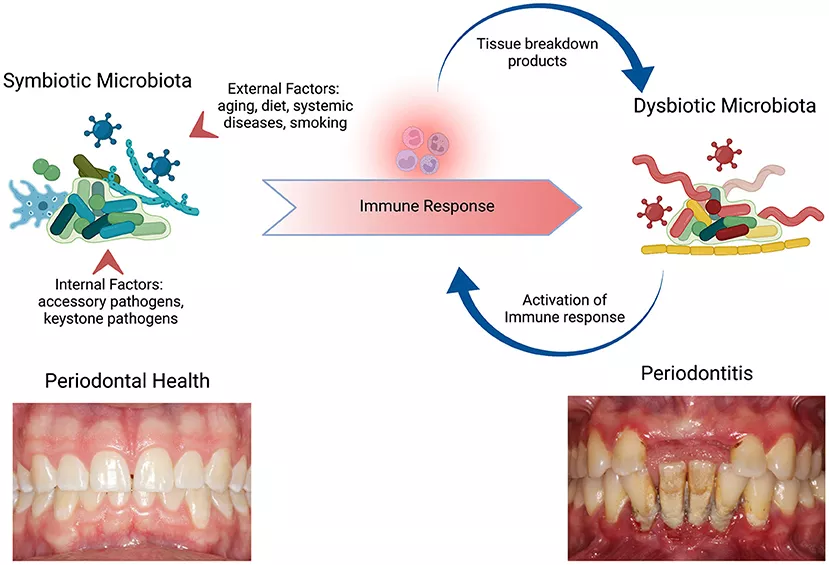
The host’s immune response to periodontal pathogens plays a dual role in periodontal disease. While it is essential for controlling bacterial infection, an exaggerated or dysregulated immune response can lead to tissue destruction.
Inflammatory mediators, such as cytokines, prostaglandins, and matrix metalloproteinases (MMPs), are released in response to bacterial challenge, leading to the breakdown of connective tissue and bone.
The Balance Between Protective and Destructive Inflammation
The current theory emphasizes the importance of the balance between protective and destructive inflammation. Protective inflammation involves the recruitment of immune cells, such as neutrophils and macrophages, which phagocytose bacteria and release antimicrobial peptides. However, when inflammation becomes chronic and dysregulated, it results in the excessive production of inflammatory mediators that contribute to tissue destruction. Understanding this balance is critical for developing therapeutic strategies aimed at modulating the host response to prevent periodontal tissue damage.
Genetic And Enviromental Factors
Genetic Susceptibility
Genetic factors play a significant role in determining an individual’s susceptibility to periodontal disease. Specific genetic polymorphisms in genes encoding components of the immune system, such as cytokines and their receptors, have been associated with an increased risk of periodontal disease. For instance, polymorphisms in the interleukin-1 (IL-1) gene cluster have been linked to a heightened inflammatory response and greater periodontal tissue destruction.
Environmental and Lifestyle Factors
Environmental and lifestyle factors, such as smoking, stress, and diet, also significantly influence the risk and progression of periodontal disease. Smoking, in particular, is a major risk factor due to its detrimental effects on the immune response and tissue healing. Nicotine and other components of tobacco smoke impair neutrophil function, reduce blood flow to the gums, and alter the microbial composition of dental plaque, thereby exacerbating periodontal disease.
The Concept of Dysbiosis
Microbial Imbalance
The current theory of periodontal disease underscores the concept of dysbiosis, which refers to an imbalance in the microbial community that leads to disease. In a healthy state, the oral microbiome is in a state of equilibrium, with beneficial and commensal bacteria maintaining a balance that prevents pathogenic overgrowth. However, factors such as poor oral hygiene, systemic diseases, and lifestyle habits can disrupt this balance, leading to the dominance of pathogenic bacteria and the onset of periodontal disease.
Biofilm and Community Interactions
Periodontal pathogens do not act alone but rather as part of a complex microbial community within the biofilm.
Interactions between different bacterial species, including synergistic and antagonistic relationships, play a crucial role in the development of dysbiosis. For example, P. gingivalis can manipulate the host immune response to create a favorable environment for other pathogenic bacteria, promoting a shift towards a dysbiotic state.
Clinical Manifestations And Diagnosis
Stages of Periodontal Disease
Periodontal disease can be broadly classified into two stages: gingivitis and periodontitis. Gingivitis is the initial, reversible stage characterized by inflammation of the gums without attachment loss. If left untreated, gingivitis can progress to periodontitis, a more severe form involving the destruction of the periodontal ligament and alveolar bone, leading to tooth mobility and eventual tooth loss.
Clinical Diagnosis
The diagnosis of periodontal disease is based on clinical and radiographic assessments. Clinicians evaluate the presence of signs such as gum inflammation, bleeding on probing, periodontal pocket depth, and attachment loss. Radiographs are used to assess bone loss around the teeth. Additionally, microbiological testing and genetic screening may be employed to identify specific pathogens and genetic markers associated with increased disease susceptibility.
Current And Emerging Therapies
Non-Surgical Treatments
Non-surgical treatments, such as scaling and root planing, are the cornerstone of periodontal therapy. These procedures involve the mechanical removal of dental plaque and calculus from tooth surfaces and periodontal pockets to reduce bacterial load and inflammation. Adjunctive therapies, such as antimicrobial agents and host modulation therapies, may be used to enhance treatment outcomes.
Surgical Interventions
In cases where non-surgical treatments are insufficient, surgical interventions may be necessary. Periodontal surgery aims to reduce pocket depths, regenerate lost tissues, and improve the overall periodontal condition. Procedures such as flap surgery, guided tissue regeneration, and bone grafting are commonly performed to achieve these goals.
Emerging Therapies and Future Directions
Emerging therapies for periodontal disease focus on targeting the underlying mechanisms of dysbiosis and inflammation.
Probiotics, prebiotics, and synbiotics are being explored for their potential to restore a healthy microbial balance.
Additionally, novel anti-inflammatory agents and immunomodulatory therapies are under investigation to modulate the host response and prevent tissue destruction. Advances in genetic and molecular research may also pave the way for personalized approaches to periodontal therapy, tailored to an individual’s genetic and microbial profile.
Conclusion
The current theory of periodontal disease highlights the intricate interplay between microbial factors, host immune response, genetic predisposition, and environmental influences. Understanding these complex interactions is essential for developing effective prevention and treatment strategies. As research continues to unravel the molecular and genetic underpinnings of periodontal disease, new therapeutic approaches hold promise for improving the management and outcomes of this prevalent and debilitating condition. Maintaining good oral hygiene, regular dental check-ups, and a healthy lifestyle remain fundamental in preventing the onset and progression of periodontal disease.