Periodontal disease, also known as gum disease, is a common condition that affects the tissues surrounding and supporting the teeth. It is a leading cause of tooth loss in adults and can have significant implications for overall health. Evaluating periodontal disease is crucial for diagnosing its severity and implementing appropriate treatments. This comprehensive article explores the methods used to evaluate periodontal disease, including clinical examinations, diagnostic tests, and patient history.
Understanding Periodontal Disease
Periodontal disease encompasses a range of inflammatory conditions affecting the gums and supporting structures of the teeth. The disease primarily progresses through two stages:
Gingivitis: This is the initial stage, characterized by inflammation of the gingiva (gums). It is often caused by the accumulation of plaque on the teeth. Gingivitis is usually reversible with good oral hygiene.
Periodontitis: If gingivitis is left untreated, it can progress to periodontitis, a more severe form of the disease that involves the loss of bone and connective tissue supporting the teeth. Periodontitis can lead to tooth mobility and loss.
How to Evaluate Periodontal Disease
1. Clinical Examination
A thorough clinical examination is the cornerstone of evaluating periodontal disease. This process involves assessing various aspects of oral health, including:
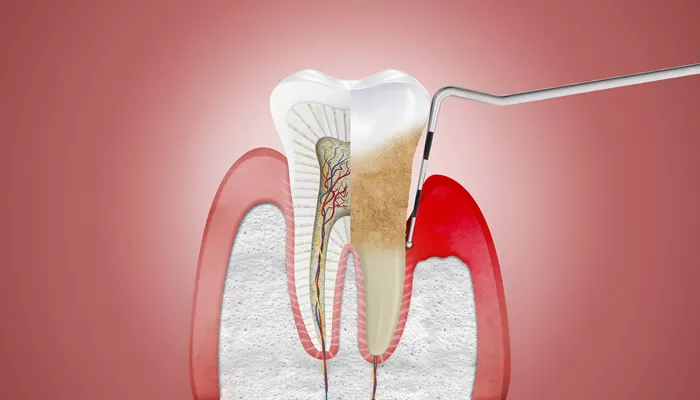
Visual Inspection: The dentist or periodontist examines the gums and teeth for signs of inflammation, such as redness, swelling, and bleeding. They also look for any visible plaque or tartar buildup.
Periodontal Probing: This involves using a specialized instrument called a periodontal probe to measure the depth of the pockets around each tooth. Healthy gums typically have pocket depths of 1 to 3 millimeters. Pocket depths greater than 4 millimeters can indicate periodontal disease.
SEE ALSO: Do Dental Implants Cure Periodontal Disease?
Attachment Level Measurement: The dentist measures the distance between the tooth’s surface and the periodontal attachment level. This measurement helps determine the extent of tissue loss.
Assessment of Gingival Recession: Gingival recession refers to the loss of gum tissue, which can expose the tooth’s root surface. This condition is assessed to evaluate the severity of the disease.
Evaluation of Tooth Mobility: Increased tooth mobility can be a sign of advanced periodontal disease. The dentist assesses the degree of mobility to determine the impact of the disease on tooth stability.
2. Diagnostic Tests
In addition to clinical examination, several diagnostic tests can aid in the evaluation of periodontal disease:
Radiographic Imaging: X-rays, including bitewing and periapical radiographs, are used to assess the bone levels around the teeth. They can reveal bone loss, which is a key indicator of periodontitis. Advanced imaging techniques, such as cone-beam computed tomography (CBCT), provide detailed 3D views of the periodontal structures.
Microbiological Testing: This test involves collecting samples from the periodontal pockets to identify specific bacteria associated with periodontal disease. The results can help tailor treatment plans based on the bacterial profile.
Genetic Testing: Genetic tests can identify individuals with a genetic predisposition to periodontal disease. These tests can provide insights into the risk factors and help in personalized treatment approaches.
Salivary Tests: Saliva can be tested for biomarkers associated with periodontal disease. Elevated levels of certain proteins or enzymes in saliva may indicate the presence or progression of the disease.
3. Patient History
A comprehensive patient history is essential in evaluating periodontal disease. Key aspects include:
Medical History: Certain medical conditions, such as diabetes and cardiovascular disease, can impact periodontal health. A detailed medical history helps identify any systemic factors contributing to periodontal disease.
Dental History: Information about previous dental treatments, oral hygiene practices, and any history of periodontal disease provides valuable context for the evaluation.
Lifestyle Factors: Factors such as smoking, diet, and stress can influence periodontal health. Understanding these lifestyle factors helps in developing a holistic treatment plan.
Risk Factors
Evaluating periodontal disease involves identifying risk factors that may contribute to its development or progression.
Common risk factors include:
Smoking: Tobacco use is a significant risk factor for periodontal disease. Smokers are more likely to develop severe forms of the disease and experience reduced healing.
Diabetes: Diabetes can impair the body’s ability to fight infections and promote inflammation, increasing the risk of periodontal disease.
Genetics: Genetic predisposition plays a role in the susceptibility to periodontal disease. Individuals with a family history of the disease may be at higher risk.
Hormonal Changes: Hormonal fose occurring during pregnancy or menopause, can affect gum health and increase the risk of periodontal disease.
Medications: Certain medications, such as antihypertensives and anticonvulsants, can impact gum health and contribute to periodontal disease.
Treatment And Management
Once periodontal disease is evaluated and diagnosed, appropriate treatment and management strategies can be implemented. Treatment may include:
Non-Surgical Therapy: This includes scaling and root planing (deep cleaning) to remove plaque and tartar from below the gumline. It also involves improving oral hygiene practices.
Surgical Therapy: In cases of advanced periodontitis, surgical interventions such as flap surgery or regenerative procedures may be necessary to restore lost tissue and bone.
Medication: Antibiotics or antimicrobial agents may be prescribed to address bacterial infections and reduce inflammation.
Ongoing Monitoring: Regular follow-up visits are essential to monitor the effectiveness of treatment and prevent recurrence.
Conclusion
Evaluating periodontal disease is a multi-faceted process that involves clinical examination, diagnostic testing, and patient history. By thoroughly assessing the severity and extent of the disease, dental professionals can develop personalized treatment plans to manage and mitigate the impact of periodontal disease. Early detection and intervention are key to preventing the progression of the disease and maintaining optimal oral health.