Periodontal disease, commonly known as gum disease, is a chronic infection that affects the tissues surrounding and supporting the teeth. It is one of the most prevalent oral health issues globally, impacting millions of people each year. The progression of periodontal disease can vary widely from individual to individual, depending on various factors such as oral hygiene habits, systemic health conditions, and genetic predisposition. One common concern among patients with periodontal disease is the lifespan of their teeth. In this comprehensive guide, we will explore the question “How long can teeth with periodontal disease live?” from a professional dental perspective, complete with subtitles and presented in an easy-to-understand, popular science style.
How Long Can Teeth with Periodontal Disease Live?
Teeth affected by periodontal disease can potentially last for a long time if the condition is caught early and managed properly. However, the longevity of these teeth depends on several factors, including the severity of the disease, the specific treatments provided, and how well the individual adheres to oral hygiene practices. Here’s a breakdown of how long teeth with periodontal disease can last under various conditions:
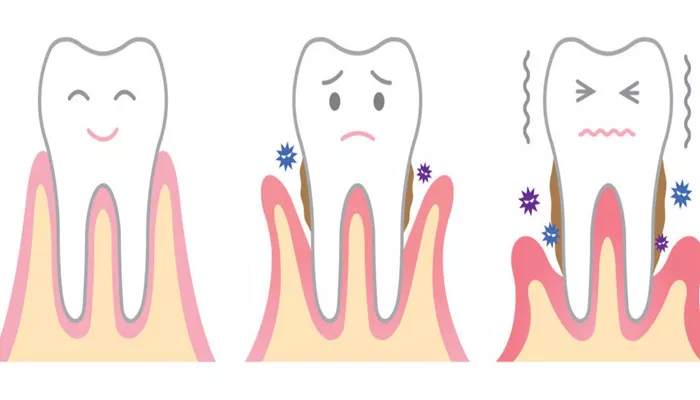
1. Early-Stage Periodontal Disease (Gingivitis)
Gingivitis, the mildest form of periodontal disease, causes inflammation of the gums but doesn’t yet affect the bone or tissues supporting the teeth. If caught early and treated with good oral hygiene (regular brushing and flossing) and professional cleanings, the damage can often be reversed.
Longevity of Teeth:
With Treatment: Teeth can last a lifetime with proper care.
Without Treatment: If gingivitis progresses to more severe periodontal disease, tooth loss is more likely.
2. Moderate Periodontal Disease
In moderate stages of periodontal disease, the infection begins to affect the tissues supporting the teeth, including the bone. Gum recession, pockets around the teeth, and bone loss may occur. Treatment typically includes scaling and root planing (deep cleaning), along with more rigorous oral hygiene and possible antibiotic treatments.
Longevity of Teeth:
With Treatment: Teeth can potentially last for many years or even decades, depending on how well the infection is controlled.
Without Treatment: If untreated, the disease may progress, leading to further bone loss and weakening of the tooth’s support, which may ultimately cause tooth mobility or loss.
3. Advanced Periodontal Disease
Advanced periodontal disease involves significant bone loss, deep pockets around the teeth, gum recession, and potential tooth mobility.
At this stage, the goal is to stop the disease’s progression and save as many teeth as possible. Surgical treatments may be necessary, including gum grafting, bone grafts, or even tooth extraction.
Longevity of Teeth:
With Treatment: Teeth may last for several more years or longer, but the prognosis depends on the severity of the bone loss and the success of the treatment.
Without Treatment: Without intervention, teeth may become increasingly loose and could eventually fall out. The risk of losing teeth increases significantly at this stage.
4. Factors That Influence Tooth Longevity
Severity of Bone Loss: The more bone loss present, the less support the teeth have, reducing their long-term survival.
Treatment Response: Teeth that respond well to treatment (such as deep cleaning or surgery) may last longer.
Oral Hygiene: Maintaining excellent oral hygiene after treatment is crucial for preventing further damage.
Lifestyle Factors: Smoking, diabetes, and other health conditions can contribute to the progression of periodontal disease, impacting tooth longevity.
Regular Dental Visits: Consistent check-ups allow for early detection of any issues and ensure that teeth remain stable.
5. Possible Tooth Loss in Advanced Cases
In severe cases of periodontal disease, even with treatment, some teeth may not be salvageable. The risk of tooth mobility (teeth becoming loose) increases as the disease progresses. In these cases, extractions may be necessary, but even then, dental implants or other restorations can be options to restore function and appearance.
Factors Affecting the Lifespan of Teeth with Periodontal Disease
The lifespan of teeth with periodontal disease can vary widely depending on several factors. Some of the most significant factors include:
Severity of Disease
The severity of periodontal disease is a critical factor in determining the lifespan of teeth. Mild cases of gingivitis may have minimal impact on the lifespan of teeth, while severe cases of periodontitis can lead to rapid bone loss and tooth loss.
Oral Hygiene Habits
Proper oral hygiene practices are essential for maintaining the health of teeth and gums. Regular brushing, flossing, and dental cleanings can help remove plaque and tartar, reducing the risk of infection and inflammation. Conversely, poor oral hygiene habits can exacerbate the progression of periodontal disease, leading to shorter tooth lifespan.
Systemic Health Conditions
Certain systemic health conditions can also affect the lifespan of teeth with periodontal disease. For example, diabetes is a well-known risk factor for periodontal disease, as it can impair the body’s ability to fight infection. Other systemic conditions, such as heart disease and respiratory infections, can also exacerbate the progression of periodontal disease.
Genetic Predisposition
Genetic factors can also play a role in the lifespan of teeth with periodontal disease. Some individuals may be more genetically predisposed to developing periodontal disease, which can impact the rate of progression and severity of symptoms.
Treatment Options for Periodontal Disease
The treatment options for periodontal disease vary depending on the severity of the disease and the individual patient’s needs. Some common treatment options include:
Non-Surgical Therapies
Non-surgical therapies are typically the first line of treatment for periodontal disease. These include:
Scaling and Root Planing: This procedure involves removing plaque and tartar from the teeth and roots, smoothing the root surfaces to prevent bacteria from adhering.
Antibiotics: Antibiotics may be prescribed to help control infection and inflammation.
Chlorhexidine Rinse: Chlorhexidine is an antiseptic rinse that can help reduce plaque and bacteria in the mouth.
Surgical Therapies
In cases of severe periodontitis, surgical therapies may be necessary to restore the health of the teeth and gums. These include:
Flap Surgery: This procedure involves lifting the gums back to clean and remove tartar and bacteria from the roots. The gums are then sutured back in place.
Bone Grafting: Bone grafting may be necessary to replace bone that has been lost due to periodontitis.
Guided Tissue Regeneration: This procedure involves placing a membrane over the exposed bone and gum tissue to encourage the growth of new bone and tissue.
Preventive Measures
Preventive measures are essential for maintaining the health of teeth and gums and reducing the risk of developing periodontal disease. Some common preventive measures include:
Regular Dental Check-Ups: Regular dental check-ups allow for early detection and treatment of periodontal disease.
Proper Oral Hygiene Practices: Regular brushing, flossing, and dental cleanings can help remove plaque and tartar, reducing the risk of infection and inflammation.
Healthy Diet: A balanced diet rich in vitamins and minerals can help support oral health.
Quit Smoking: Smoking is a significant risk factor for periodontal disease and should be avoided.
Conclusion
The lifespan of teeth with periodontal disease can vary widely depending on several factors, including the severity of the disease, oral hygiene habits, systemic health conditions, and genetic predisposition. Proper treatment and preventive measures are essential for maintaining the health of teeth and gums and reducing the risk of tooth loss. While periodontal disease is a chronic condition that requires ongoing management, with proper care, many patients can maintain their teeth for many years.
Related topics: