Dental implants are a revolutionary method in oral restoration that involves placing artificial tooth roots into the jawbone to support and secure the restoration of missing teeth. However, in some cases, the jawbone may not have sufficient bone mass or quality to support the placement of dental implants. In such scenarios, bone grafts become necessary to augment the jawbone and provide a stable foundation for the implants. This article aims to provide a detailed introduction to the sources of bone grafts used in dental implant surgery from a professional perspective.
Introduction to Bone Grafts for Dental Implants
Bone grafts are surgical procedures that involve adding bone tissue to an area where it is needed to enhance its structure and stability. In dental implant surgery, bone grafts are often used to increase the bone mass and density in the jawbone, enabling the successful placement and integration of dental implants. The sources of bone grafts for dental implants can be categorized into several types, each with its own unique characteristics and applications.
Sources of Bone Grafts
1. Autogenous Bone Grafts (Autografts)
Autogenous bone grafts, also known as autografts, involve harvesting bone tissue from the patient’s own body. This type of bone graft is considered the most ideal due to its excellent biocompatibility and ability to integrate seamlessly with the existing bone.
Intraoral Sources: Common intraoral sources for autogenous bone grafts include the chin, mandibular ramus, and maxillary tuberosity. These areas typically provide sufficient bone material with minimal surgical morbidity.
Extraoral Sources: Extraoral sources for autogenous bone grafts include the iliac crest, rib, and tibia. These sources are often used when larger volumes of bone are required. However, they may involve more significant surgical morbidity and longer recovery times.
The advantages of autogenous bone grafts include fast bone healing, minimal immune rejection, and high osteogenic potential. However, they also have disadvantages such as the need for additional surgical sites, potential for donor site morbidity, and increased surgical complexity.
2. Allogeneic Bone Grafts (Allografts)
Allogeneic bone grafts, also known as allografts, involve using bone tissue donated by another person. These grafts undergo rigorous processing and sterilization to ensure their safety and effectiveness.
Processing: Donated bone tissue undergoes high-temperature inactivation of DNA, demineralization, and irradiation sterilization to convert it into a safe and effective graft material.
Allogeneic bone grafts offer the advantage of reducing the need for harvesting bone from the patient’s own body, thereby minimizing donor site morbidity. However, their biocompatibility may be slightly inferior to autogenous bone, and they may take longer to integrate with the host bone.
3. Xenogeneic Bone Grafts (Xenografts)
Xenogeneic bone grafts, also known as xenografts, involve using bone tissue from a different species, typically cows. These grafts undergo extensive processing to remove all organic material and undergo demineralization to enhance their biocompatibility.
Applications: Xenografts are widely used in clinical practice due to their abundance and cost-effectiveness. They are particularly useful in guiding the growth of autologous bone.
The advantages of xenografts include their wide availability, cost-effectiveness, and ability to stimulate autologous bone growth. However, their integration with the host bone may be slightly inferior to autogenous and allogeneic bone grafts.
4. Alloplastic Bone Grafts (Synthetic Grafts)
Alloplastic bone grafts, also known as synthetic grafts, involve using artificial materials such as hydroxyapatite, tricalcium phosphate, and other calcium phosphate-based ceramics.
Advantages: Synthetic grafts offer the advantage of being readily available, easy to use, and having predictable outcomes. They can be tailored to match the patient’s specific needs and provide a stable scaffold for bone regeneration.
Disadvantages: However, synthetic grafts may lack the osteogenic potential of autogenous and allogeneic bone grafts, and their integration with the host bone may be slower.
The Process of Bone Grafting for Dental Implants
The process of bone grafting for dental implants typically involves several steps:
Assessment and Planning: The surgeon assesses the patient’s jawbone structure using imaging techniques such as computed tomography (CT) scans to determine the amount and type of bone grafting needed.
Harvesting the Bone Graft: Depending on the chosen bone graft source, the surgeon harvests the bone tissue from the appropriate site. For autogenous bone grafts, this may involve an additional surgical procedure. For allogeneic, xenogeneic, or alloplastic bone grafts, the material is prepared and ready for use.
Preparing the Recipient Site: The surgeon prepares the recipient site in the jawbone by creating a bed that is suitable for the bone graft. This may involve removing damaged or infected bone tissue and shaping the site to accept the graft.
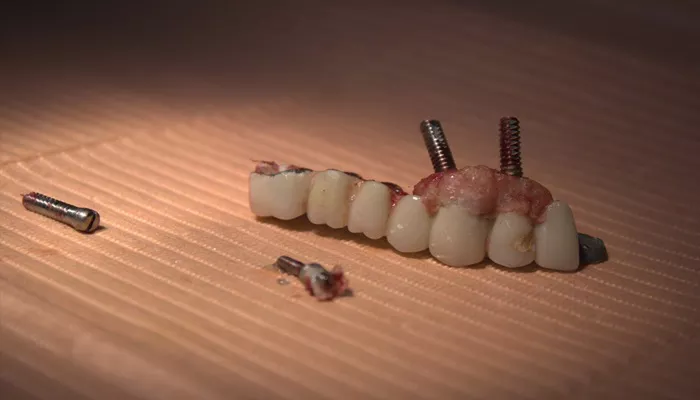
Placing the Bone Graft: The surgeon places the bone graft into the prepared site and secures it in place using screws, plates, or other fixation devices if necessary.
Healing and Integration: Over time, the bone graft integrates with the surrounding bone tissue through a process called osseointegration. This process can take several months, during which the patient may need to follow specific post-operative instructions and attend follow-up appointments for monitoring.
Implant Placement: Once the bone graft has successfully integrated with the surrounding bone, the surgeon can proceed with placing the dental implant. This involves drilling a hole in the bone at the desired location, inserting the implant, and securing it in place.
Considerations for Bone Grafting
When considering bone grafting for dental implants, several factors need to be taken into account:
Patient’s Overall Health: The patient’s overall health, including any medical conditions or medications they are taking, can affect the healing process and the success of the bone graft.
Amount of Bone Loss: The amount of bone loss determines the type and amount of bone grafting needed. Severe bone loss may require more extensive grafting procedures.
Jawbone Density and Quality: The density and quality of the jawbone affect the ability of the bone graft to integrate and support the dental implant. Poor bone quality may require additional treatment or the use of special implants.
Cost and Insurance Coverage: The cost of bone grafting can vary depending on the type of graft used, the complexity of the procedure, and the geographical location. Patients should check with their insurance provider to determine if the procedure is covered.
Conclusion
Bone grafts are an essential part of dental implant surgery, providing a stable foundation for the successful placement and integration of implants. The sources of bone grafts for dental implants include autogenous, allogeneic, xenogeneic, and alloplastic bone grafts, each with its own unique characteristics and applications. When considering bone grafting, patients should work closely with their oral surgeon to determine the most appropriate type of graft based on their individual needs and circumstances. By understanding the sources and processes involved in bone grafting for dental implants, patients can make informed decisions about their oral health and achieve optimal outcomes.
Related topics: