Periodontal disease and diabetes are two significant health issues that can affect millions of people worldwide. Research has shown a strong connection between these two conditions. Understanding this link is crucial for effective prevention, management, and treatment. This article will explore the relationship between periodontal disease and diabetes, how they influence each other, and the importance of maintaining good oral health for individuals with diabetes.
Understanding Periodontal Disease
What Is Periodontal Disease?
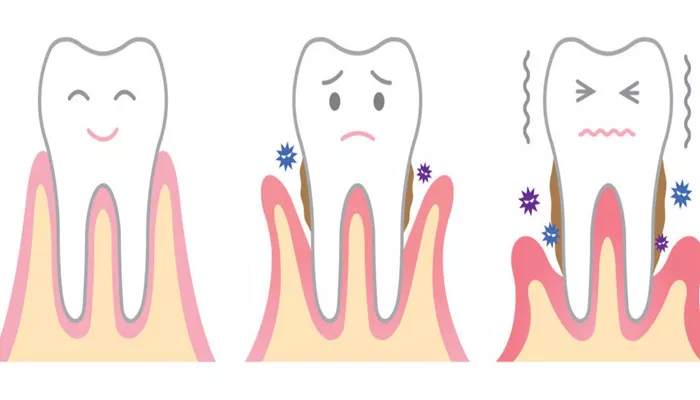
Periodontal disease, also known as gum disease, is an inflammatory condition that affects the tissues surrounding the teeth. It begins with gingivitis, characterized by red, swollen gums that may bleed. If left untreated, gingivitis can progress to periodontitis, a more severe form that involves loss of bone and tissue supporting the teeth.
Causes of Periodontal Disease
The primary cause of periodontal disease is the accumulation of plaque, a sticky film of bacteria that forms on teeth. Other factors that contribute to periodontal disease include:
Poor Oral Hygiene: Inadequate brushing and flossing can lead to plaque buildup.
Smoking: Tobacco use is a significant risk factor for gum disease.
Hormonal Changes: Hormonal fluctuations can affect gum health.
Genetic Factors: Some individuals may be genetically predisposed to gum disease.
Symptoms of Periodontal Disease
Common symptoms of periodontal disease include:
- Red, swollen gums
- Gums that bleed during brushing or flossing
- Bad breath
- Loose teeth or shifting teeth
- Tooth sensitivity
Understanding Diabetes
What Is Diabetes?
Diabetes is a chronic condition that occurs when the body cannot properly regulate blood sugar (glucose) levels. There are two main types of diabetes:
Type 1 Diabetes: An autoimmune condition where the body does not produce insulin.
Type 2 Diabetes: A more common form where the body becomes resistant to insulin or does not produce enough insulin.
Causes of Diabetes
The causes of diabetes vary depending on the type:
Type 1 Diabetes: The exact cause is unclear, but it involves an autoimmune response that attacks insulin-producing cells in the pancreas.
Type 2 Diabetes: This type is often linked to lifestyle factors, such as obesity, physical inactivity, and poor diet.
Symptoms of Diabetes
Common symptoms of diabetes include:
- Increased thirst and hunger
- Frequent urination
- Fatigue
- Blurred vision
- Slow-healing wounds
The Link Between Periodontal Disease and Diabetes
Bidirectional Relationship
Research has established a bidirectional relationship between periodontal disease and diabetes. This means that not only can diabetes increase the risk of developing periodontal disease, but periodontal disease can also worsen diabetes control.
How Diabetes Affects Periodontal Disease
Increased Inflammation: Diabetes can lead to chronic inflammation in the body. This inflammation can exacerbate the inflammatory response in the gums, making them more susceptible to infection.
Impaired Blood Flow: Diabetes can cause damage to blood vessels, reducing blood flow to the gums. This can hinder the healing process and increase the risk of gum disease.
Altered Immune Response: Individuals with diabetes may have a weakened immune response. This makes it harder for the body to fight off infections, including those in the gums.
High Blood Sugar Levels: Elevated blood sugar levels can lead to an increase in the amount of glucose in the saliva. This creates an environment that promotes the growth of harmful bacteria, contributing to periodontal disease.
How Periodontal Disease Affects Diabetes
Inflammatory Response: The bacteria in periodontal disease can trigger an inflammatory response throughout the body.
This inflammation can interfere with insulin function, making it more challenging to control blood sugar levels.
Increased Insulin Resistance: Periodontal disease may contribute to increased insulin resistance, a condition where the body’s cells do not respond effectively to insulin. This can lead to higher blood sugar levels.
Worsened Glycemic Control: Studies have shown that individuals with periodontal disease may have more difficulty controlling their blood sugar levels. This can lead to complications associated with diabetes.
Potential Complications: Poorly controlled diabetes can lead to various complications, including cardiovascular disease, kidney problems, and nerve damage. The presence of periodontal disease can further complicate these issues.
Managing the Link Between Periodontal Disease and Diabetes
Importance of Oral Health for Diabetic Patients
For individuals with diabetes, maintaining good oral health is crucial. Here are some key strategies:
Regular Dental Check-Ups: Diabetic patients should visit the dentist regularly for check-ups and cleanings. This helps in the early detection and treatment of periodontal disease.
Good Oral Hygiene Practices: Daily brushing and flossing are essential. Using an antimicrobial mouthwash can also help reduce bacteria in the mouth.
Monitoring Blood Sugar Levels: Keeping blood sugar levels within the target range can help reduce the risk of developing periodontal disease.
Healthy Lifestyle Choices: A balanced diet, regular exercise, and avoiding tobacco are vital for managing both diabetes and periodontal health.
Treatment Options for Periodontal Disease in Diabetic Patients
If a diabetic patient develops periodontal disease, treatment options may include:
Scaling and Root Planing: This deep cleaning procedure removes plaque and tartar from below the gumline, helping to reduce inflammation and infection.
Antibiotics: In some cases, antibiotics may be prescribed to control bacterial infection in the gums.
Surgical Treatments: For advanced periodontal disease, surgical options may be necessary to restore gum health and bone support.
Ongoing Maintenance Care: Regular periodontal maintenance visits are essential for monitoring gum health and preventing recurrence.
Conclusion
The link between periodontal disease and diabetes is significant and complex. Each condition can influence the other, leading to a cycle of worsening health. For individuals with diabetes, maintaining good oral health is essential for managing their condition and preventing complications. Regular dental visits, proper oral hygiene, and healthy lifestyle choices are crucial steps in breaking the cycle of periodontal disease and diabetes. By understanding this relationship, patients can take proactive measures to protect their oral and overall health. If you have diabetes, it is important to consult with both your healthcare provider and dentist to develop a comprehensive plan for managing your health.
Related topics: