Refractory periodontal disease is a complex and challenging oral health condition. It refers to a type of periodontal disease that does not respond to standard treatment methods. This condition can lead to severe gum and tooth issues if not managed properly. In this article, we will explore what refractory periodontal disease is, its causes, symptoms, diagnosis, treatment options, and prevention strategies.
Understanding Periodontal Disease
What Is Periodontal Disease?
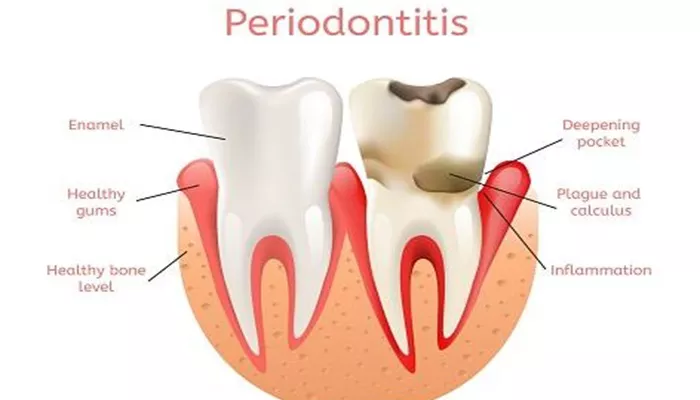
Periodontal disease, commonly known as gum disease, is an infection of the tissues surrounding the teeth. It begins with the buildup of plaque, a sticky film of bacteria that forms on the teeth. If plaque is not removed through proper oral hygiene, it can harden into tartar, leading to inflammation of the gums (gingivitis). If untreated, gingivitis can progress to more severe forms of periodontal disease, including refractory periodontal disease.
Stages of Periodontal Disease
Periodontal disease progresses through several stages:
Gingivitis: This is the earliest stage, characterized by swollen and bleeding gums. At this stage, there is no loss of bone or tissue.
Mild Periodontal Disease: This stage involves some loss of attachment and bone around the teeth, along with increased gum inflammation.
Moderate Periodontal Disease: In this stage, there is further loss of attachment and more significant inflammation.
Severe Periodontal Disease: This is the most advanced stage, characterized by extensive loss of attachment and bone, leading to tooth mobility and potential tooth loss.
Refractory Periodontal Disease: This is a specific category where the disease does not respond to conventional treatments, despite proper oral hygiene and professional care.
What Causes Refractory Periodontal Disease?
Bacterial Infection
The primary cause of refractory periodontal disease is the presence of harmful bacteria in the mouth. These bacteria produce toxins that irritate the gums and lead to inflammation. In refractory cases, the bacteria may be particularly aggressive or resistant to treatment.
Risk Factors
Several factors can contribute to the development of refractory periodontal disease:
Poor Oral Hygiene: Inadequate brushing and flossing can lead to plaque buildup, increasing the risk of periodontal disease.
Genetics: Some individuals may be genetically predisposed to periodontal disease, making them more susceptible to its refractory form.
Smoking: Tobacco use significantly increases the risk of developing periodontal disease and can hinder healing.
Chronic Diseases: Conditions such as diabetes, autoimmune diseases, and certain hormonal changes can affect gum health and contribute to refractory cases.
Certain Medications: Medications that cause dry mouth or alter the immune response can increase the risk of periodontal disease.
Poor Nutrition: A diet lacking essential nutrients can weaken the immune system and make it harder for the body to fight infections.
Symptoms of Refractory Periodontal Disease
Common Symptoms
Refractory periodontal disease presents several symptoms that may indicate the need for dental evaluation. These symptoms include:
Persistent Bad Breath: Ongoing bad breath that does not improve with regular oral hygiene can be a sign of periodontal disease.
Swollen and Bleeding Gums: Gums may appear red, swollen, and bleed during brushing or flossing.
Receding Gums: Gums may pull away from the teeth, exposing more of the tooth root.
Pocket Formation: Spaces (pockets) may form between the teeth and gums, indicating loss of attachment.
Tooth Mobility: Teeth may become loose due to loss of supporting bone.
Potential Complications
If left untreated, refractory periodontal disease can lead to severe complications, including:
Tooth Loss: Advanced periodontal disease can result in the loss of teeth.
Abscess Formation: Infections can lead to painful abscesses in the gums.
Systemic Health Issues: Periodontal disease has been linked to other health conditions, such as heart disease and diabetes.
Diagnosing Refractory Periodontal Disease
Dental Examination
To diagnose refractory periodontal disease, a dentist will perform a thorough dental examination. This examination typically includes:
Visual Inspection: The dentist will look for signs of gum inflammation, bleeding, and pocket formation.
Periodontal Probing: A periodontal probe will be used to measure the depth of gum pockets around each tooth. Pocket depths greater than 4 millimeters may indicate periodontal disease.
Dental X-rays: X-rays may be taken to assess bone loss around the teeth.
Periodontal Charting
Periodontal charting is a systematic way to record the health of the gums and the depth of the pockets. This information helps the dentist determine the severity of the disease and develop an appropriate treatment plan.
Treatment Options for Refractory Periodontal Disease
Non-Surgical Treatments
The first line of treatment for refractory periodontal disease typically involves non-surgical options, including:
Professional Cleaning (Scaling and Root Planing): This procedure involves removing plaque and tartar from the teeth and smoothing the root surfaces to promote healing. Scaling removes plaque and tartar above and below the gum line, while root planing smooths the tooth roots to help the gums reattach.
Antibiotic Therapy: In some cases, dentists may prescribe antibiotics to help control bacterial infection. This can include topical antibiotics applied directly to the gums or oral antibiotics taken by mouth.
Improved Oral Hygiene Practices: Patients will receive guidance on improving their oral hygiene routine at home. This includes proper brushing and flossing techniques, as well as the use of antibacterial mouthwash.
Surgical Treatments
If non-surgical treatments are not effective, surgical options may be considered. These include:
Flap Surgery (Pocket Reduction Surgery): This procedure involves lifting the gums away from the teeth to remove tartar and bacteria from deep pockets. The gums are then sutured back into place, reducing pocket depth.
Bone Grafting: If bone loss has occurred, bone grafting may be necessary to restore lost bone. This involves placing bone material in the area to encourage new bone growth.
Guided Tissue Regeneration: This technique involves placing a barrier between the bone and gum tissue to allow the bone to regenerate and support the teeth.
Laser Therapy: Some dentists may use laser technology to remove infected tissue and promote healing.
Prevention of Refractory Periodontal Disease
Good Oral Hygiene Practices
Maintaining good oral hygiene is crucial for preventing refractory periodontal disease. Key practices include:
Brushing Twice Daily: Use a soft-bristled toothbrush and fluoride toothpaste to brush your teeth for at least two minutes.
Flossing Daily: Flossing helps remove plaque and food particles from between the teeth and below the gum line.
Using Mouthwash: An antibacterial mouthwash can help reduce plaque and gingivitis.
Regular Dental Visits
Regular dental check-ups are essential for maintaining oral health. It is recommended to visit the dentist every six months for a professional cleaning and examination. Early detection and treatment of gum disease can prevent progression to more severe stages.
Healthy Lifestyle Choices
Making healthy lifestyle choices can also help prevent periodontal disease:
Quit Smoking: If you smoke, seek help to quit. This can significantly improve your gum health.
Eat a Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins supports overall health and oral health.
Manage Chronic Conditions: If you have conditions like diabetes, work with your healthcare provider to manage them effectively.
Conclusion
Refractory periodontal disease is a serious condition that requires prompt attention and treatment. Understanding its causes, symptoms, and treatment options is essential for maintaining good oral health. By practicing good oral hygiene, visiting the dentist regularly, and making healthy lifestyle choices, you can prevent refractory periodontal disease and protect your gums and teeth. If you notice any signs of gum disease, do not hesitate to seek professional help. Early intervention is key to preventing more severe complications and ensuring a healthy smile for years to come.
Related topics: