Dental implants are a popular choice for replacing missing teeth. They provide a strong foundation for crowns, bridges, or dentures. However, some patients may experience bleeding around their dental implants. This can be concerning and may indicate an underlying problem. In this article, we will explore the reasons why dental implants may bleed, the implications of this bleeding, and what steps you can take to address the issue.
Understanding Dental Implants
What Are Dental Implants?
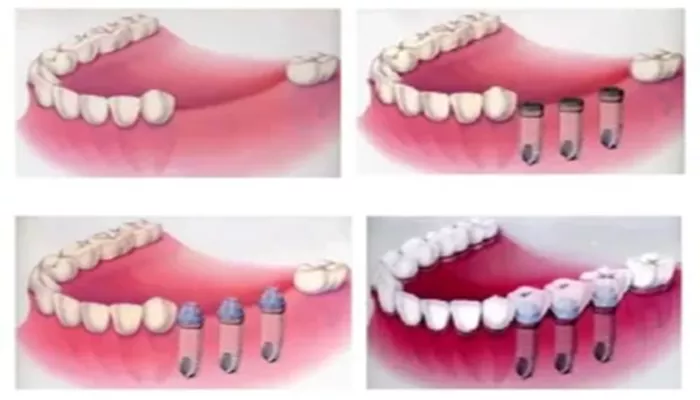
Dental implants are artificial tooth roots made from biocompatible materials, typically titanium. They are surgically placed into the jawbone to support crowns, bridges, or dentures. The main components of a dental implant system include:
Implant Screw: The titanium post that is inserted into the jawbone.
Abutment: A connector that sits on top of the implant screw and holds the crown or bridge.
Crown: The visible part of the tooth that is placed on the abutment.
Why Are Dental Implants Used?
Dental implants serve several important purposes:
Replacing Missing Teeth: They restore function, allowing patients to eat and speak normally.
Preventing Bone Loss: Implants stimulate the jawbone, preventing the bone loss that often occurs after tooth extraction.
Improving Aesthetics: They provide a natural-looking solution for missing teeth.
Reasons Why Dental Implants May Bleed
1. Poor Oral Hygiene
One of the most common reasons for bleeding around dental implants is poor oral hygiene. When plaque and tartar build up around the implant, it can lead to inflammation of the gums, known as peri-implant mucositis. Symptoms of this condition include:
- Red, swollen gums
- Bleeding when brushing or flossing
- Bad breath
If left untreated, peri-implant mucositis can progress to a more severe condition called peri-implantitis.
2. Peri-implantitis
Peri-implantitis is an inflammatory condition that affects the tissues surrounding the dental implant. It is similar to gum disease and can lead to infection and bone loss. Signs of peri-implantitis include:
- Bleeding around the implant
- Swelling and redness of the gums
- Pus or discharge from the implant site
- Increased mobility of the implant
If you experience bleeding and other symptoms of peri-implantitis, it is crucial to contact your dentist for evaluation and treatment.
3. Gum Recession
Gum recession can expose the underlying implant or abutment, leading to bleeding. When the gums recede, they can become inflamed and more susceptible to infection. Factors that contribute to gum recession include:
Periodontal Disease: Existing gum disease can lead to the loss of gum tissue.
Aggressive Brushing: Brushing too hard can damage the gums and cause them to recede.
Genetics: Some individuals are more prone to gum recession due to genetic factors.
4. Mechanical Factors
Mechanical factors can also contribute to bleeding around dental implants. These may include:
Overloading the Implant: Excessive force on the implant, such as grinding teeth (bruxism) or having an improper bite, can cause stress on the implant and surrounding tissues, leading to inflammation and bleeding.
Defective Components: If the implant screw, abutment, or crown is defective or improperly placed, it can lead to irritation and bleeding.
5. Infection
Infection is a significant concern when it comes to dental implants. If bacteria enter the implant site, it can lead to inflammation and bleeding. Signs of infection include:
- Persistent bleeding around the implant
- Swelling and redness of the gums
- Pain or discomfort in the area
If you suspect an infection, it is essential to seek prompt dental care to prevent further complications.
6. Post-Surgical Complications
Bleeding may occur after the initial placement of the dental implant. This can be a normal part of the healing process.
However, excessive or prolonged bleeding may indicate a complication. Possible causes of post-surgical bleeding include:
Blood Thinners: If you are taking blood-thinning medications, you may be at a higher risk for bleeding.
Surgical Technique: In some cases, the surgical technique used may lead to complications, including bleeding.
If you experience significant bleeding after implant surgery, contact your dentist immediately.
7. Systemic Health Issues
Certain systemic health issues can affect the healing process and contribute to bleeding around dental implants. These may include:
Diabetes: Uncontrolled diabetes can impair healing and increase the risk of infection.
Blood Disorders: Conditions that affect blood clotting can lead to increased bleeding.
Autoimmune Diseases: Some autoimmune diseases can affect gum health and increase the risk of inflammation.
If you have a systemic health condition, discuss it with your dentist to ensure proper management during and after implant placement.
Implications of Bleeding Around Dental Implants
Aesthetic Concerns
Bleeding around dental implants can lead to aesthetic concerns. If the gums are inflamed and bleeding, it can affect the overall appearance of your smile. Healthy gums should be pink and firm, not red and swollen.
Health Risks
Bleeding around dental implants can indicate underlying health issues that may lead to more serious complications if left untreated. These complications can include:
- Bone loss around the implant
- Implant failure
- Increased risk of systemic infections
It is essential to address any bleeding around your dental implants promptly to prevent these risks.
What to Do If Your Implants Bleed
1. Maintain Good Oral Hygiene
The first step in addressing bleeding around dental implants is to maintain good oral hygiene. Follow these tips to improve your oral care routine:
Brush Twice Daily: Use a soft-bristled toothbrush to gently clean around the implant.
Floss Daily: Use dental floss or interdental brushes to remove plaque and food particles around the implant.
Use Antibacterial Mouthwash: Rinse with an antibacterial mouthwash to reduce the risk of infection.
2. Schedule a Dental Appointment
If you notice bleeding around your dental implants, it is essential to schedule an appointment with your dentist. They can evaluate the situation and determine the cause of the bleeding. Early intervention can prevent more severe complications.
3. Discuss Treatment Options
If your dentist diagnoses peri-implantitis or another condition, they may recommend treatment options such as:
Professional Cleaning: A thorough cleaning to remove plaque and tartar buildup around the implant.
Antibiotics: If an infection is present, your dentist may prescribe antibiotics to help control it.
Surgical Intervention: In severe cases, surgical treatment may be necessary to address bone loss or other complications.
4. Consider Gum Grafting
If gum recession is a contributing factor to the bleeding, your dentist may recommend a gum graft. This procedure involves taking tissue from another part of your mouth and attaching it to the receded area. Gum grafting can help restore the gum line and improve the health of your gums.
5. Address Underlying Health Conditions
If you have underlying health conditions that may contribute to bleeding, work with your healthcare provider to manage them effectively. Keeping conditions like diabetes under control can improve your overall oral health and reduce the risk of complications.
6. Avoid Smoking and Tobacco Use
If you smoke or use tobacco products, consider quitting. Smoking can impair healing and increase the risk of gum disease and implant failure. Discuss cessation programs with your healthcare provider if needed.
Preventing Bleeding Around Dental Implants
1. Choose an Experienced Dentist
Selecting a qualified and experienced dentist or oral surgeon is crucial for the success of your dental implants. They will ensure proper placement and follow-up care.
2. Follow Post-Operative Instructions
After receiving dental implants, follow all post-operative care instructions provided by your dentist. This includes:
Taking prescribed medications as directed.
Attending all follow-up appointments.
3. Maintain Regular Dental Check-Ups
Regular dental check-ups are essential for monitoring the health of your dental implants. Your dentist can identify potential issues early and provide necessary treatment.
4. Practice Good Oral Hygiene
Good oral hygiene is vital for the longevity and health of dental implants. Ensure you brush and floss regularly and use mouthwash as recommended by your dentist.
Conclusion
Experiencing bleeding around dental implants can be alarming. However, understanding the potential causes and knowing what to do can help you address the issue effectively. Common reasons for bleeding include poor oral hygiene, peri-implantitis, gum recession, mechanical factors, infection, post-surgical complications, and systemic health issues.
If you notice bleeding around your dental implants, contact your dentist immediately. They can assess the situation and recommend the best course of action. By maintaining good oral hygiene and addressing any underlying issues, you can help ensure the long-term success and health of your dental implants. Remember, dental implants are designed to provide a lasting solution for missing teeth, and with proper care, you can enjoy the benefits of your implants for years to come.
Related topics: