Dental implants are a popular solution for replacing missing teeth, offering a durable and aesthetically pleasing option for many patients. However, like any surgical procedure, dental implants come with potential risks, including infections.
Infections around dental implants, known as peri-implant infections, can lead to serious complications if not addressed promptly. This article will explore how to treat infections around dental implants, including prevention strategies, signs of infection, treatment options, and the importance of maintaining good oral hygiene.
Introduction to Dental Implants and Infections
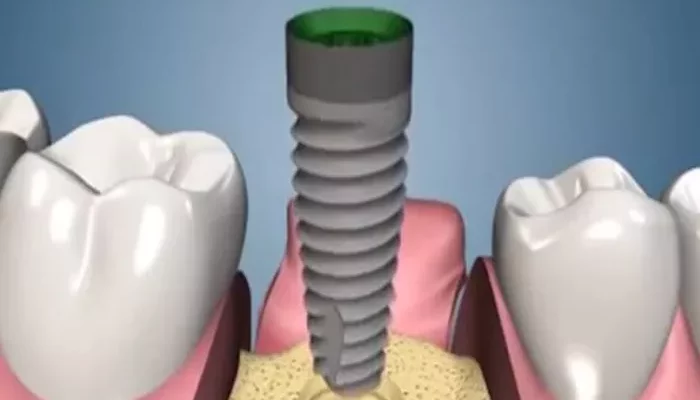
Dental implants consist of titanium posts that are surgically placed into the jawbone to serve as artificial tooth roots. Once integrated with the bone, they can support crowns, bridges, or dentures. While dental implants have a high success rate, infections can occur at any stage of the process, from the initial surgery to the healing phase and beyond.
Peri-implant infections can manifest as peri-implant mucositis or peri-implantitis. Mucositis refers to inflammation of the soft tissues around the implant without bone loss, while peri-implantitis involves both inflammation of the soft tissue and loss of the supporting bone. Early detection and treatment are crucial to prevent further complications, including implant failure.
Signs And Symptoms of Infection
Recognizing the signs of infection around dental implants is vital for prompt treatment. Common symptoms include:
1. Redness and Swelling
Inflammation of the gums around the implant site is often the first sign of infection. The gums may appear red and swollen, indicating irritation or infection.
2. Pain and Discomfort
Patients may experience pain or discomfort around the implant. This pain can range from mild to severe and may worsen when pressure is applied to the area.
3. Bleeding
Gums that bleed during brushing or flossing can indicate an infection. Bleeding may also occur spontaneously without any apparent cause.
4. Pus or Discharge
The presence of pus or a foul-smelling discharge around the implant site is a clear indication of infection. This discharge may be yellow or green and can be accompanied by a bad taste in the mouth.
5. Mobility of the Implant
If the implant feels loose or mobile, it may indicate a severe infection affecting the bone support around the implant. This is a concerning sign that requires immediate attention.
6. Bad Breath
Persistent bad breath (halitosis) can be a symptom of infection. The bacteria present in the infected area can produce foul-smelling compounds, leading to unpleasant odors.
Causes of Infections Around Dental Implants
Understanding the causes of infections around dental implants can help in prevention and treatment. Common causes include:
1. Poor Oral Hygiene
Inadequate brushing and flossing can lead to the accumulation of plaque and bacteria around the implant, increasing the risk of infection. Proper oral hygiene is essential for maintaining the health of the implant and surrounding tissues.
2. Smoking
Smoking can impair healing and reduce blood flow to the gums, making it more difficult for the body to fight infections.
Smokers are at a higher risk of developing peri-implant infections.
3. Pre-existing Periodontal Disease
Patients with a history of gum disease are more susceptible to infections around dental implants. Periodontal disease can compromise the health of the gums and bone, increasing the risk of complications.
4. Surgical Complications
Infections can also arise from complications during the surgical placement of the implant. Contamination during the procedure or improper placement can lead to infection.
5. Systemic Health Issues
Certain systemic health conditions, such as diabetes or autoimmune disorders, can impair the body’s ability to heal and fight infections. Patients with these conditions should be closely monitored for signs of infection.
Treatment Options for Infections Around Dental Implants
If an infection is suspected, it is essential to seek professional dental care promptly. Treatment options may vary based on the severity of the infection and the underlying causes.
1. Professional Cleaning
A thorough professional cleaning by a dentist or dental hygienist is often the first step in treating an infection. This cleaning removes plaque and tartar buildup around the implant and helps reduce inflammation.
2. Antibiotic Therapy
In many cases, antibiotics are prescribed to help eliminate the infection. The choice of antibiotic will depend on the specific bacteria causing the infection. It is crucial to complete the entire course of antibiotics as prescribed, even if symptoms improve before finishing the medication.
3. Antiseptic Rinses
Dentists may recommend antiseptic mouth rinses to help reduce bacteria in the mouth. These rinses can aid in the healing process and provide additional support in managing the infection.
4. Surgical Intervention
In severe cases where the infection has led to significant bone loss or if there is an abscess, surgical intervention may be necessary. This may involve:
Flap Surgery: The dentist may perform flap surgery to access the infected area, clean the site, and remove any infected tissue. The gums are then sutured back in place for healing.
Bone Grafting: If bone loss has occurred, a bone graft may be necessary to restore the supporting structure around the implant. This procedure involves placing bone material (either from the patient or a donor) to encourage new bone growth.
5. Removal of the Implant
In rare cases where the infection cannot be controlled or if the implant is severely compromised, the dentist may recommend removing the implant. This decision is typically a last resort, as it can impact future treatment options.
Prevention Strategies for Infections Around Dental Implants
Preventing infections around dental implants is crucial for long-term success. Here are effective strategies to reduce the risk of infection:
1. Maintain Good Oral Hygiene
Practicing excellent oral hygiene is the cornerstone of preventing infections. Patients should:
Brush their teeth at least twice a day using a soft-bristled toothbrush.
Floss daily to remove plaque from around the implant and between teeth.
Use an antibacterial mouthwash to help reduce bacteria in the mouth.
2. Regular Dental Check-ups
Regular dental visits for professional cleanings and check-ups are essential for monitoring the health of dental implants.
Dentists can identify potential issues early and provide necessary treatment.
3. Quit Smoking
Quitting smoking can significantly improve oral health and overall healing. Patients should seek support and resources to help them stop smoking, especially before and after implant surgery.
4. Manage Systemic Health Conditions
Patients with systemic health issues, such as diabetes, should work closely with their healthcare providers to manage their conditions effectively. Good control of these conditions can enhance healing and reduce the risk of infections.
5. Follow Post-operative Instructions
After dental implant surgery, it is crucial to follow all post-operative care instructions provided by the dentist. This includes guidelines for oral hygiene, diet, and activity levels during the healing process.
Conclusion
Infections around dental implants can pose significant challenges, but with prompt recognition and appropriate treatment, they can often be managed effectively. Understanding the signs and symptoms of infection, the causes, and the available treatment options is essential for anyone considering or already having dental implants.
Preventive measures play a critical role in maintaining the health of dental implants and reducing the risk of infections. By practicing good oral hygiene, attending regular dental check-ups, and managing overall health, patients can enjoy the long-term benefits of their dental implants.
Related topics: