Dental implants have emerged as a revolutionary solution for replacing missing teeth, offering patients a durable and natural-looking alternative to traditional dentures or bridges. While dental implants are generally considered safe and effective, like any medical procedure, they come with potential risks and negative effects that patients should understand.
This comprehensive article explores in detail the various negative effects associated with dental implants, ranging from common issues to rare complications, providing valuable insights for informed decision-making.
What Is Dental Implants?
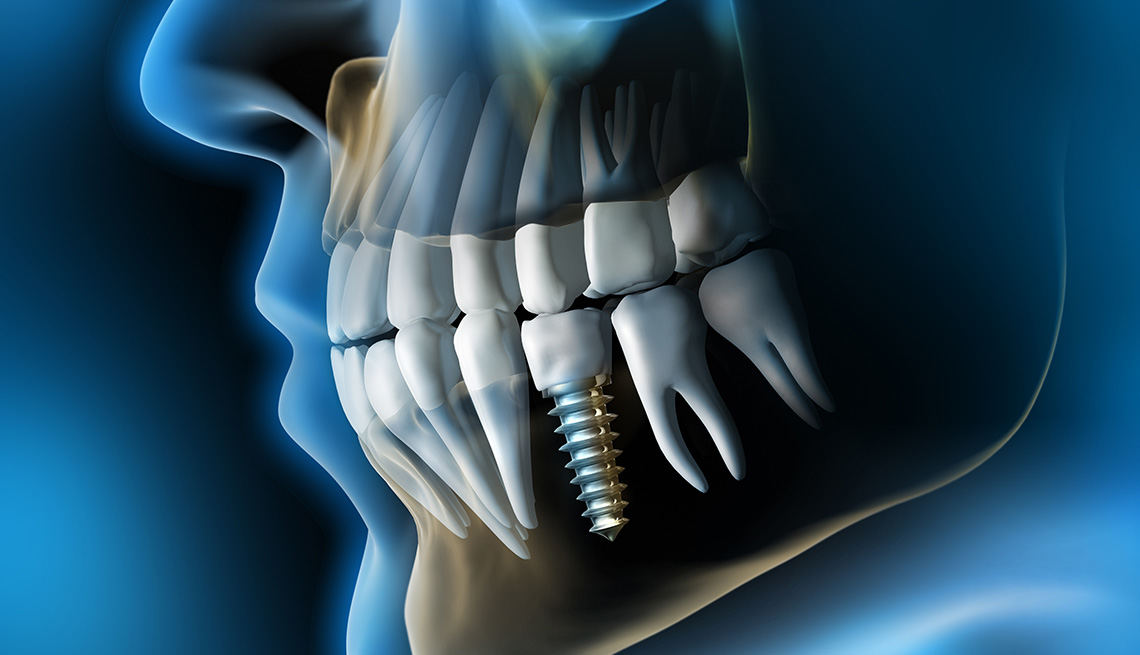
Dental implants are artificial tooth roots typically made of biocompatible materials such as titanium, surgically placed into the jawbone to support replacement teeth or dental prostheses. They offer several advantages over conventional tooth replacement options, including improved stability, functionality, and aesthetics. Despite their numerous benefits, it’s essential for patients to be aware of the potential drawbacks and complications that may arise from dental implant treatment.
see also: 5 Tips for Keeping Your Dental Implants And Gums Clean
Common Negative Effects of Dental Implants
Surgical Risks and Complications:
Dental implant surgery, though routine and well-practiced, carries inherent risks similar to any surgical procedure. These risks include infection at the implant site, damage to surrounding structures (such as nerves or blood vessels), and excessive bleeding. While these complications are relatively rare, they underscore the importance of choosing a skilled and experienced dental implant specialist.
Pain and Discomfort:
Post-operative pain and discomfort are common following dental implant placement. Patients may experience swelling, bruising, and soreness around the implant site, which typically resolves within a few days to weeks. Pain management strategies, including prescribed medications and cold compresses, can help alleviate these symptoms during the initial recovery period.
Gum and Tissue Issues:
In some cases, patients may experience complications related to the gums and surrounding tissues. This can include gum recession, inflammation (gingivitis or peri-implantitis), or irritation around the implant area. These issues may arise due to poor oral hygiene practices, inadequate implant care, or improper placement of the implant. Regular dental visits and meticulous oral hygiene routines are crucial for preventing and managing these complications.
Implant Failure:
While modern dental implants boast high success rates (typically around 95-98%), there is a small risk of implant failure.
Implant failure can occur if the implant does not properly fuse with the jawbone (osseointegration) or if it becomes loose over time. Factors contributing to implant failure include smoking, uncontrolled diabetes, insufficient bone density, or systemic health conditions that impair healing.
Nerve Damage:
During implant placement, there is a slight risk of nerve damage in the surrounding areas, leading to temporary or, in rare cases, permanent numbness or tingling sensations in the lips, gums, chin, or tongue. This risk is minimized through careful pre-operative planning, advanced imaging techniques, and precise surgical techniques.
Less Common Complications
Sinus Issues:
Dental implants placed in the upper jaw, particularly in the posterior regions, may protrude into the sinus cavities. This can potentially lead to sinusitis (sinus infection) or discomfort. Proper assessment of sinus anatomy through diagnostic imaging (such as panoramic X-rays or CT scans) helps minimize this risk, along with appropriate surgical techniques to avoid sinus perforation.
Allergic Reactions:
Although rare, some individuals may develop allergic reactions to the materials used in dental implants, particularly titanium alloys or other components. Allergic responses can manifest as localized swelling, rash, itching, or discomfort around the implant site. Patients with known metal allergies should undergo thorough allergy testing prior to implant placement or consider alternative materials.
Bone Resorption:
Over time, the bone supporting a dental implant may undergo resorption (bone loss), compromising the stability and longevity of the implant. This can occur due to peri-implantitis (inflammation around the implant), inadequate bone quality or quantity, or excessive mechanical forces on the implant. Regular dental examinations and proactive management of peri-implant health are essential for minimizing bone loss and preserving implant function.
Implant Fracture or Mechanical Failure:
Although rare, dental implants can fracture or experience mechanical failure under extreme conditions, such as trauma or excessive occlusal forces. This may necessitate implant replacement or repair to restore function and aesthetics effectively.
Long-term Considerations and Patient Education
Maintenance and Oral Hygiene:
Proper maintenance of dental implants is crucial for their long-term success. Patients should adhere to meticulous oral hygiene practices, including regular brushing, flossing, and the use of antimicrobial mouth rinses to prevent plaque buildup and inflammation around implants.
Cost Considerations:
Dental implants represent a significant investment in oral health. Patients should consider not only the initial cost of implant treatment but also potential long-term maintenance expenses, including routine dental visits, professional cleanings, and potential future treatments for implant-related complications.
Conclusion
In conclusion, while dental implants offer substantial benefits in restoring oral function and aesthetics, they are not without potential risks and negative effects. Patients considering implant treatment should undergo thorough consultation and evaluation by a qualified dental professional to assess candidacy, discuss potential risks, and establish realistic expectations.