Periodontal disease is a significant oral health concern that affects millions of individuals worldwide. It is characterized by inflammation and infection of the supporting structures of the teeth, which can lead to tooth loss if not properly managed.
One of the critical indicators of periodontal disease is the measurement of pocket depth around the teeth. Understanding what constitutes a healthy pocket depth versus one that indicates periodontal disease is essential for both prevention and treatment.
What Is Periodontal Pockets?
Periodontal pockets are spaces that form between the teeth and the gums due to the breakdown of the supporting structures caused by bacterial infection. In a healthy mouth, the gums fit snugly around the teeth, creating a shallow crevice typically measuring between 1 and 3 millimeters (mm). When the gums become inflamed due to plaque accumulation, they can begin to pull away from the teeth, leading to the formation of deeper pockets.
Pocket Depth Measurements
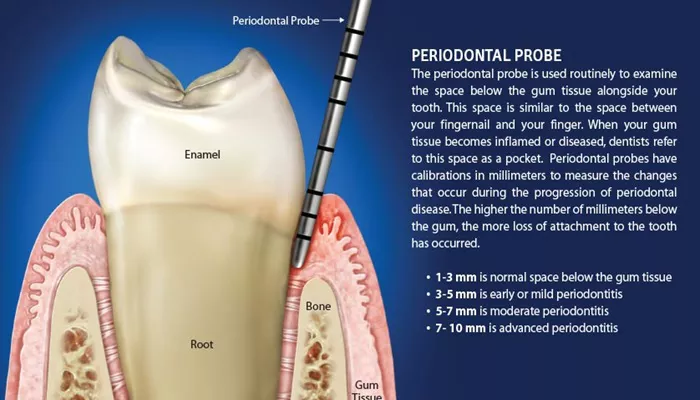
The measurement of pocket depth is performed using a dental instrument called a periodontal probe. This probe is gently inserted into the space between the gum and tooth to assess how deep the pocket is. The depth of these pockets is categorized as follows:
1 to 3 mm: This range is considered normal and healthy. The gums are firmly attached to the teeth, and there is no significant inflammation or infection.
4 to 5 mm: Pockets in this range indicate early or mild periodontitis. This suggests the presence of gum disease, and while it may not be severe, it requires attention and intervention.
5 to 7 mm: This depth signifies moderate periodontitis. The condition is more advanced, and there is a greater risk of further tissue loss and complications.
7 mm or more: Pockets measuring this depth indicate advanced periodontitis. At this stage, significant damage to the supporting structures of the teeth has occurred, and aggressive treatment is necessary to prevent tooth loss.
SEE ALSO: When Is Bone Graft Needed for Periodontal Disease?
The Importance of Pocket Depth in Diagnosis
The measurement of pocket depth is a vital component of diagnosing periodontal disease. Dentists often perform a thorough examination of the gums, looking for signs of inflammation, bleeding, and the presence of plaque or tartar. The depth of the pockets helps determine the severity of the disease and guides the treatment plan.
In addition to pocket depth, dentists may also utilize dental X-rays to assess bone loss around the teeth, which is another critical factor in diagnosing the extent of periodontal disease.
What Causes Periodontal Pockets?
Periodontal pockets develop primarily due to the accumulation of plaque—a sticky film of bacteria that forms on the teeth.
If not removed through regular brushing and flossing, plaque can harden into tartar, which can only be removed through professional dental cleaning. When plaque and tartar build up, they irritate the gum tissue, leading to inflammation and the formation of pockets.
Several factors can contribute to the development of periodontal disease and the deepening of pockets, including:
Poor oral hygiene: Inadequate brushing and flossing allow plaque to accumulate.
Smoking: Tobacco use significantly increases the risk of gum disease.
Hormonal changes: Conditions such as pregnancy and menopause can affect gum health.
Certain medical conditions: Diseases like diabetes and autoimmune disorders can impact the body’s ability to fight infections.
Genetic predisposition: Some individuals may be more susceptible to gum disease due to their genetic makeup.
Signs And Symptoms of Periodontal Disease
Recognizing the signs of periodontal disease is crucial for early intervention. Common symptoms include:
Red, swollen, or bleeding gums: Healthy gums should not bleed during brushing or flossing.
Persistent bad breath: Foul-smelling breath can indicate an underlying infection.
Receding gums: If the gums are pulling away from the teeth, this may indicate the presence of pockets.
Loose teeth: Advanced periodontal disease can lead to tooth mobility due to bone loss.
Changes in bite: A shift in how the teeth fit together can signal gum disease.
Diagnosis of Periodontal Disease
To diagnose periodontal disease, a dental professional will typically follow these steps:
Medical history review: Understanding the patient’s overall health and any risk factors for gum disease.
Visual examination: Inspecting the gums for signs of inflammation, bleeding, and plaque buildup.
Pocket depth measurement: Using a periodontal probe to assess the depth of pockets around each tooth.
X-rays: Taking radiographs to evaluate bone loss around the teeth.
Assessment of gum attachment: Determining how well the gums are attached to the teeth.
Treatment Options for Periodontal Disease
The treatment for periodontal disease varies depending on the severity of the condition and the depth of the pockets.
Options include:
Non-surgical treatments:
Scaling and root planing: This deep cleaning procedure involves removing plaque and tartar from below the gumline and smoothing the tooth roots to promote healing.
Antibiotics: Topical or oral antibiotics may be prescribed to help control bacterial infection.
Surgical treatments:
Flap surgery: In cases of advanced periodontitis, this procedure involves lifting the gums to clean the tooth roots and reshape the bone if necessary.
Bone grafting: If significant bone loss has occurred, grafting may be performed to restore bone structure.
Conclusion
Understanding pocket depth is crucial in recognizing and managing periodontal disease. A pocket depth of 4 mm or greater is typically indicative of gum disease, with deeper pockets signaling more advanced stages of the condition. Early diagnosis and treatment are vital in preventing further complications and preserving oral health. By maintaining good oral hygiene practices and seeking regular dental care, individuals can significantly reduce their risk of developing periodontal disease and ensure a healthy smile for years to come.