Dental health is crucial for overall well-being, and two of the most common dental issues people face are caries and periodontal disease.
While both conditions can lead to significant oral health problems, they are distinct in their causes, symptoms, and treatments. Understanding the differences between caries and periodontal disease is essential for effective prevention and management.
In this article, we will explore what caries and periodontal disease are, their causes, symptoms, treatment options, and preventive measures.
By the end, you will have a clearer understanding of these two dental conditions and how to maintain optimal oral health.
What Are Dental Caries?
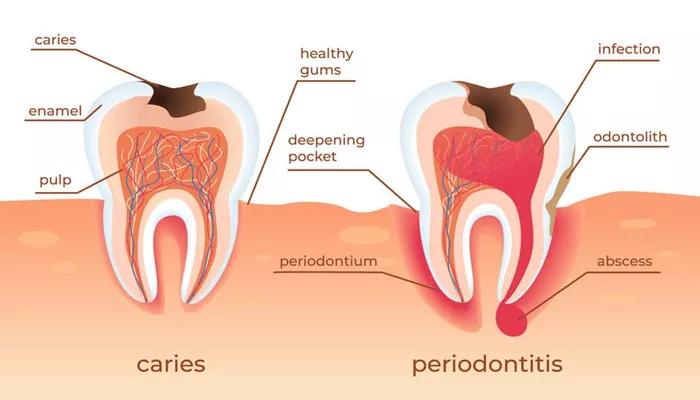
Dental caries, commonly known as cavities, is a disease that affects the hard tissues of the teeth. It is characterized by the demineralization of tooth enamel, leading to the formation of holes or cavities. Caries is a widespread condition that can affect people of all ages.
Causes of Dental Caries
Caries develops when bacteria in the mouth produce acids that attack the tooth enamel. The primary factors contributing to the development of caries include:
Bacterial Plaque: Dental plaque is a sticky film of bacteria that forms on the teeth. When sugars from food and beverages are consumed, bacteria in the plaque metabolize these sugars and produce acids.
Poor Oral Hygiene: Inadequate brushing and flossing allow plaque to accumulate, increasing the risk of caries.
Diet: A diet high in sugars and carbohydrates can promote the growth of bacteria that cause caries. Frequent snacking and sugary drinks can also contribute to the problem.
Fluoride Deficiency: Fluoride helps strengthen tooth enamel and makes it more resistant to acid attacks. A lack of fluoride can increase the risk of caries.
Dry Mouth: Saliva helps neutralize acids and wash away food particles. Conditions that cause dry mouth can lead to an increased risk of caries.
SEE ALSO: How to Shrink Gum Pockets Naturally?
Symptoms of Dental Caries
The symptoms of dental caries can vary depending on the severity of the condition. Early stages may not present noticeable symptoms, but as caries progress, the following signs may occur:
Tooth Sensitivity: Increased sensitivity to hot, cold, or sweet foods and beverages.
Visible Holes or Pits: Cavities may appear as small holes or pits on the surface of the teeth.
Toothache: Pain in the affected tooth, which may be sharp or throbbing.
Discoloration: Dark spots or discoloration on the tooth surface.
Treatment of Dental Caries
The treatment for dental caries depends on the severity of the condition:
Fluoride Treatments: In the early stages of caries, fluoride treatments can help remineralize the enamel and reverse the decay process.
Dental Fillings: For cavities that have formed, the dentist will remove the decayed portion of the tooth and fill it with a dental material, such as composite resin or amalgam.
Crowns: If the tooth is extensively damaged, a crown may be placed to restore its shape and function.
Root Canal Treatment: If the decay has reached the pulp of the tooth, a root canal may be necessary to remove the infected tissue.
Tooth Extraction: In severe cases where the tooth cannot be saved, extraction may be required.
What Is Periodontal Disease?
Periodontal disease, also known as gum disease, is an inflammatory condition that affects the tissues surrounding and supporting the teeth. It is primarily caused by the accumulation of plaque and tartar on the teeth and gums. Periodontal disease can range from mild gingivitis to severe periodontitis.
Causes of Periodontal Disease
The primary cause of periodontal disease is the buildup of plaque and tartar on the teeth. Factors that contribute to the development of periodontal disease include:
Bacterial Infection: The presence of harmful bacteria in dental plaque can lead to inflammation of the gums.
Poor Oral Hygiene: Inadequate brushing and flossing allow plaque to accumulate, increasing the risk of gum disease.
Smoking and Tobacco Use: Tobacco products can impair blood flow to the gums and hinder healing, increasing the risk of periodontal disease.
Hormonal Changes: Hormonal fluctuations during puberty, menstruation, pregnancy, and menopause can make gums more sensitive and susceptible to disease.
Medical Conditions: Certain medical conditions, such as diabetes and autoimmune diseases, can increase the risk of periodontal disease.
Symptoms of Periodontal Disease
The symptoms of periodontal disease can vary depending on the severity of the condition:
Red, Swollen Gums: Gums may appear inflamed and bleed easily during brushing or flossing.
Bad Breath: Persistent bad breath (halitosis) may occur due to bacterial infection.
Receding Gums: Gums may pull away from the teeth, leading to tooth sensitivity and exposure of tooth roots.
Loose Teeth: Advanced periodontal disease can cause teeth to become loose or shift.
Pus Between Teeth and Gums: Pus may be present in the pockets between the teeth and gums.
Treatment of Periodontal Disease
The treatment for periodontal disease depends on the severity of the condition:
Professional Cleaning: In the early stages, a dental hygienist will perform a thorough cleaning to remove plaque and tartar buildup.
Scaling and Root Planing: For moderate to severe cases, scaling and root planing may be necessary. This deep cleaning procedure removes plaque and tartar from below the gumline and smooths the tooth roots.
Antibiotics: Antibiotic treatments may be prescribed to help control bacterial infection.
Surgical Procedures: In advanced cases, surgical procedures such as flap surgery or bone grafting may be necessary to restore periodontal health.
Maintenance: Regular dental check-ups and cleanings are essential for maintaining gum health and preventing recurrence.
Key Differences Between Caries And Periodontal Disease
While both caries and periodontal disease are common dental problems, they differ significantly in several aspects:
1. Nature of the Condition
Caries: Affects the hard tissues of the teeth, leading to decay and the formation of cavities.
Periodontal Disease: Affects the soft tissues surrounding the teeth, leading to inflammation and potential tooth loss.
2. Causes
Caries: Primarily caused by bacterial acid production from sugars in the diet.
Periodontal Disease: Caused by the accumulation of plaque and tartar, leading to bacterial infection and inflammation.
3. Symptoms
Caries: Symptoms include tooth sensitivity, visible holes, toothache, and discoloration.
Periodontal Disease: Symptoms include red, swollen gums, bad breath, receding gums, and loose teeth.
4. Treatment Approaches
Caries: Treatment typically involves fluoride treatments, fillings, crowns, root canals, or extractions.
Periodontal Disease: Treatment may include professional cleaning, scaling and root planing, antibiotics, and surgical procedures.
5. Prevention Strategies
Caries: Prevention focuses on good oral hygiene, reducing sugar intake, and using fluoride products.
Periodontal Disease: Prevention emphasizes regular dental cleanings, good oral hygiene, and avoiding tobacco products.
Conclusion
Understanding the differences between caries and periodontal disease is essential for maintaining good oral health. Both conditions can lead to significant dental problems if left untreated, but they require different approaches for prevention and treatment. By practicing good oral hygiene, visiting the dentist regularly, and making healthy dietary choices, individuals can reduce their risk of both caries and periodontal disease.