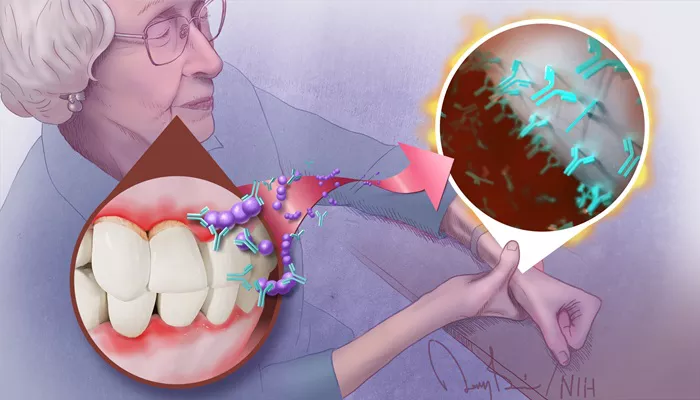
Tokyo [Japan], September 8 (ANI): Periodontal disease, which affects the gums and tissues surrounding the teeth, is one of the most widespread dental disorders globally. Caused primarily by the buildup of bacterial biofilm around the teeth, this condition can lead to tooth loss if left untreated. Beyond its impact on oral health, periodontal disease has been linked to broader systemic effects, raising concerns about its role in other health issues.
Clinical research over several decades has shown a connection between the periodontal pathogen Aggregatibacter actinomycetemcomitans (A. actinomycetemcomitans) and the onset and worsening of rheumatoid arthritis (RA), a severe autoimmune condition affecting the joints. Despite this knowledge, the molecular mechanisms behind this relationship have remained largely unclear.
In a recent study published on August 15, 2024, in the International Journal of Oral Science, researchers from Tokyo Medical and Dental University (TMDU) in Japan aimed to address this gap. Their detailed investigation focused on how the bacteria responsible for periodontal disease can contribute to the progression of RA, using an animal model to study the underlying processes.
The team first conducted preliminary experiments to determine whether infection with A. actinomycetemcomitans would exacerbate arthritis in mice. Using a well-established collagen antibody-induced arthritis mouse model, which mirrors several aspects of RA in humans, the researchers discovered that infection with this bacterium resulted in increased swelling of the limbs, greater infiltration of immune cells into the joint lining, and elevated levels of the inflammatory cytokine interleukin-1b (IL-1b).
Interestingly, the study found that these arthritis symptoms could be alleviated through the use of clodronate, a chemical compound that depletes macrophages, a type of immune cell. This indicated that macrophages play a significant role in worsening RA when the body is infected with A. actinomycetemcomitans.
Further research using macrophages derived from mouse bone marrow revealed that A. actinomycetemcomitans infection led to an increase in IL-1b production. This, in turn, activated a multiprotein complex called the inflammasome, which is critical in initiating the body’s inflammatory response to infections.
To solidify their findings, the researchers used caspase-11-deficient mice, which lack a key protein involved in inflammasome activation. In these mice, the activation of the inflammasome due to A. actinomycetemcomitans was significantly reduced, and they experienced less severe arthritis symptoms. This suggests that caspase-11 plays a pivotal role in the worsening of RA linked to this bacterial infection.
“Our research provides new insights into the connection between periodontal bacteria and the aggravation of arthritis via inflammasome activation, shedding light on the long-debated relationship between periodontal disease and systemic illnesses,” said Professor Toshihiko Suzuki, one of the study’s lead authors.
The researchers hope that their findings will contribute to the development of new therapeutic approaches to manage RA.
“These results may lead to advances in clinical treatments for RA caused by A. actinomycetemcomitans infection. By targeting inflammasome activation, we could reduce inflammation in the joints and help alleviate arthritis symptoms,” said Dr. Tokuju Okano, the study’s lead author.
Looking ahead, the research team is optimistic that their work could extend beyond arthritis treatment. “Our findings might also support the development of therapies for other systemic diseases, such as Alzheimer’s disease, which has also been linked to periodontal bacteria,” added Dr. Okano.