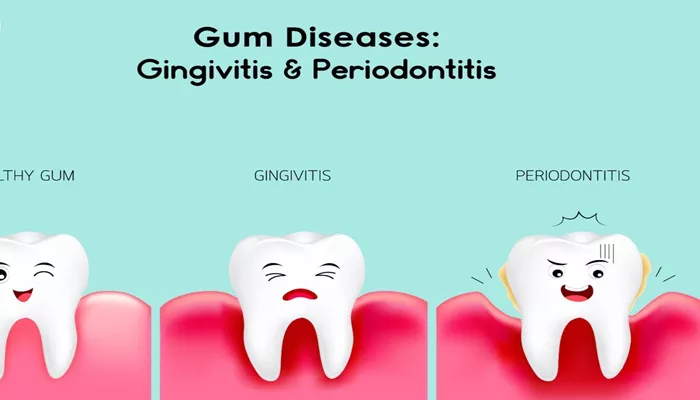
Gum disease is a prevalent condition that affects a significant portion of the population. Among the various forms of gum disease, gingivitis and periodontitis are the most common. While they are often mentioned together, they represent different stages of gum disease, each with distinct characteristics, causes, and consequences. This article aims to clarify the differences between gingivitis and periodontitis, providing a detailed overview of their symptoms, causes, treatments, and preventive measures.
What Are Gingivitis And Periodontitis?
Gingivitis is the initial stage of gum disease characterized by inflammation of the gums. It is typically caused by the accumulation of plaque—a sticky film of bacteria that forms on teeth. When plaque is not removed through regular brushing and flossing, it can irritate the gum tissue, leading to symptoms such as redness, swelling, and bleeding during brushing.
Periodontitis, on the other hand, is a more advanced form of gum disease that occurs when gingivitis is left untreated. It involves inflammation that extends beyond the gums to the underlying bone and connective tissue that support the teeth.
This stage can lead to the formation of pockets between the teeth and gums, which can become infected, resulting in further tissue and bone loss.
Key Differences Between Gingivitis And Periodontitis
| Feature | Gingivitis | Periodontitis |
| Definition | Inflammation of the gums | Advanced gum disease affecting bones |
| Symptoms | Swollen, red gums; bleeding during brushing | Gum recession; pockets between teeth; loose teeth |
| Reversibility | Typically reversible with proper care | Not fully reversible; may require surgical intervention |
| Bone Loss | No bone loss occurs | Bone loss is common |
| Treatment | Professional cleaning, improved oral hygiene | Deep cleaning, possible surgery, antibiotics |
| Associated Risks | Generally low | Higher risk of tooth loss and systemic health issues |
Causes of Gingivitis And Periodontitis
Both gingivitis and periodontitis share similar causes, primarily related to poor oral hygiene. However, certain factors can contribute to the progression from gingivitis to periodontitis.
Common Causes of Gingivitis:
Plaque Buildup: The primary cause of gingivitis is the accumulation of plaque on teeth.
Poor Oral Hygiene: Inconsistent brushing and flossing allow plaque to harden into tartar, which irritates the gums.
Smoking and Tobacco Use: These habits can impair gum health and increase the risk of gingivitis.
Hormonal Changes: Changes during puberty, menstruation, pregnancy, or menopause can make gums more sensitive.
Certain Medications: Some medications can reduce saliva flow, increasing the risk of gum disease.
Common Causes of Periodontitis:
Untreated Gingivitis: If gingivitis is not treated, it can progress to periodontitis.
Genetics: A family history of gum disease can increase susceptibility.
Chronic Conditions: Diseases such as diabetes, heart disease, and autoimmune disorders can exacerbate gum issues.
Poor Nutrition: A diet low in vitamins and minerals can impair gum health.
Stress: Stress can affect the body’s immune response, making it harder to fight infections.
Symptoms of Gingivitis and Periodontitis
Recognizing the symptoms of both conditions is crucial for early intervention.
Symptoms of Gingivitis:
Red, swollen gums
Bleeding gums during brushing or flossing
Tenderness in the gums
Symptoms of Periodontitis:
Persistent bad breath
Gums that bleed easily
Gum recession, leading to longer-looking teeth
Formation of pockets between teeth and gums
Loose teeth or changes in bite alignment
Diagnosis of Gingivitis And Periodontitis
Diagnosis typically involves a dental examination, where a dentist will assess the health of your gums and may use a probe to measure pocket depths around the teeth.
Gingivitis is usually diagnosed based on visual inspection and patient-reported symptoms.
Periodontitis requires more detailed examination, including X-rays to evaluate bone loss and pocket depth measurements.
Treatment Options
Treating Gingivitis:
The treatment for gingivitis is straightforward and focuses on improving oral hygiene:
Professional Cleaning: A dental hygienist will remove plaque and tartar from teeth.
Improved Oral Hygiene: Regular brushing (twice daily) and flossing (daily) are essential.
Antimicrobial Mouthwash: This can help reduce bacteria in the mouth.
Treating Periodontitis:
Treatment for periodontitis is more complex and may include:
Scaling and Root Planing: A deep cleaning procedure that removes plaque and tartar from below the gum line.
Antibiotics: These may be prescribed to help control bacterial infection.
Surgical Treatments: In severe cases, procedures like flap surgery or bone grafts may be necessary to restore gum health.
Regular Maintenance: Ongoing dental cleanings and check-ups are crucial to manage periodontitis.
Preventive Measures
Preventing both gingivitis and periodontitis is largely about maintaining good oral hygiene:
Brush Twice Daily: Use fluoride toothpaste and a soft-bristled toothbrush.
Floss Daily: Clean between teeth to remove plaque and food particles.
Regular Dental Check-ups: Visit the dentist at least twice a year for professional cleanings and examinations.
Healthy Diet: Consume a balanced diet rich in vitamins and minerals to support gum health.
Avoid Tobacco: Quitting smoking and avoiding tobacco products can significantly reduce the risk of gum disease.
Conclusion
Understanding the differences between gingivitis and periodontitis is essential for maintaining oral health. While gingivitis is a reversible condition, periodontitis can lead to serious complications if not treated promptly.