Periodontal disease is a significant public health concern affecting millions of individuals worldwide. It encompasses a group of inflammatory conditions that impact the supporting structures of the teeth, including the gums, periodontal ligaments, and alveolar bone. Understanding how to classify periodontal disease is essential for effective diagnosis and treatment. The classification system helps dental professionals communicate about the disease, assess its severity, and plan appropriate interventions.
In this article, we will explore the various classifications of periodontal diseases in detail. We will discuss the different forms of periodontal disease, their characteristics, and how they are categorized. This comprehensive overview aims to clarify the classification system for both dental professionals and patients.
Classification of Periodontal Diseases
The classification of periodontal diseases can be broadly divided into two main categories: gingival diseases and periodontitis. Each category contains specific subtypes that reflect the clinical presentation and underlying pathophysiology.
1. Gingival Diseases
Gingival diseases are primarily characterized by inflammation of the gingival tissues. They can be classified into two main types:
Dental Plaque-Induced Gingivitis
This form results from the accumulation of dental plaque and is reversible with proper oral hygiene. It is characterized by:
- Redness
- Swelling
- Bleeding upon probing
Non-Dental Plaque-Induced Gingivitis
This category includes gingival diseases that are not directly related to plaque accumulation. Examples include:
- Allergic reactions
- Viral infections (e.g., herpes simplex)
- Hormonal changes (e.g., pregnancy gingivitis)
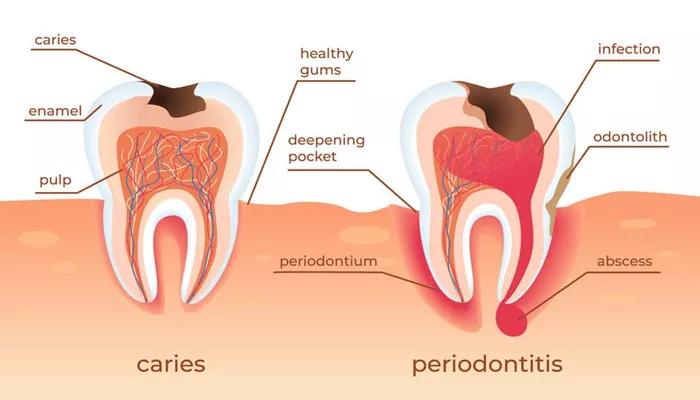
2. Periodontitis
Periodontitis is a more severe condition that involves inflammation and destruction of the supporting structures of the teeth. The classification of periodontitis has evolved significantly, particularly with the introduction of a multi-dimensional staging and grading system.
Staging of Periodontitis
Staging refers to the severity of periodontitis at presentation and is divided into four stages:
Stage I: Initial Periodontitis
- Mild inflammation
- Probing depths ≤ 4 mm
- No tooth loss
Stage II: Moderate Periodontitis
- Probing depths ≤ 5 mm
- Clinical attachment loss (CAL) ≤ 3-4 mm
- Horizontal bone loss
Stage III: Severe Periodontitis
- Probing depths ≥ 6 mm
- CAL ≥ 5 mm
- Possible tooth loss (0-4 teeth)
Stage IV: Very Severe Periodontitis
- Probing depths ≥ 6 mm
- CAL ≥ 5 mm
- Significant tooth loss (>5 teeth)
Grading of Periodontitis
Grading provides additional information about the rate of disease progression and risk factors associated with periodontitis.
There are three grades:
Grade A: Slow Progression
No significant attachment loss over time
Low risk factors (e.g., non-smoker)
Grade B: Moderate Progression
Some attachment loss observed
Moderate risk factors (e.g., smoking <10 cigarettes/day)
Grade C: Rapid Progression
Significant attachment loss within a short period
High-risk factors (e.g., uncontrolled diabetes)
3. Specific Forms of Periodontitis
Within the broader classification of periodontitis, there are several specific forms recognized:
Necrotizing Periodontal Diseases
These are characterized by tissue necrosis and include:
- Necrotizing Ulcerative Gingivitis (NUG)
- Painful ulcers on the gums
- Associated with stress or immunosuppression
- Necrotizing Ulcerative Periodontitis (NUP)
- Similar to NUG but involves deeper structures leading to bone loss
Aggressive Periodontitis
Previously classified separately, aggressive periodontitis is now included under general periodontitis but is characterized by rapid attachment loss and bone destruction, often occurring in younger individuals.
Chronic Periodontitis
The most common form, chronic periodontitis typically affects adults and is characterized by:
- Slow progression
- Presence of periodontal pockets
Endodontic-Periodontal Lesions
These lesions occur when there is a pathological connection between endodontic (pulpal) issues and periodontal disease, often complicating treatment.
Periodontal Abscesses
Acute localized infections that result in pus accumulation within the periodontal tissues, leading to rapid tissue destruction.
Conclusion
Classifying periodontal diseases is crucial for effective diagnosis and treatment planning in dental practice. The current classification system provides a comprehensive framework that incorporates staging and grading to reflect the complexity and severity of these conditions accurately.
In summary, periodontal disease classification has evolved significantly over time, reflecting advances in our understanding of these complex conditions. By utilizing this multi-dimensional approach, dental professionals can enhance patient outcomes through informed decision-making in diagnosis and treatment planning.
Related topics: