Periodontal disease is a common dental condition that affects millions of people worldwide. It is primarily caused by the accumulation of plaque, which harbors various bacteria. However, identifying the specific pathogens responsible for periodontal disease can be challenging. This article will explore the reasons why the pathogens of periodontal disease are difficult to identify, the implications of this difficulty, and potential strategies for better understanding these pathogens.
Understanding Periodontal Disease
What Is Periodontal Disease?
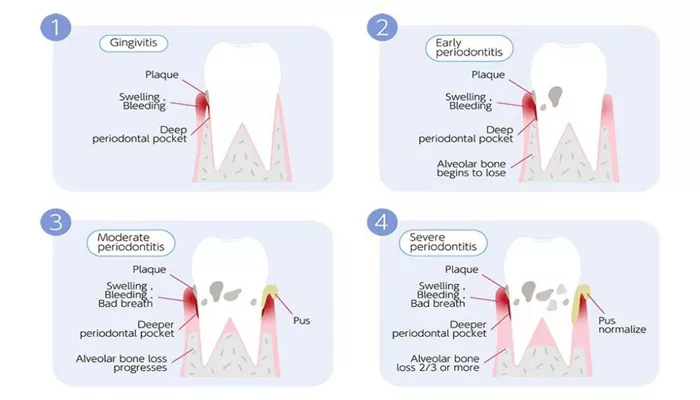
Periodontal disease refers to the inflammation and infection of the tissues surrounding the teeth. It begins with gingivitis, characterized by swollen and bleeding gums. If left untreated, it can progress to periodontitis, where the infection spreads to the supporting structures of the teeth, including the bone. This can lead to tooth loss and other serious health issues.
Common Symptoms
Symptoms of periodontal disease include:
- Red, swollen gums
- Bleeding when brushing or flossing
- Bad breath
- Loose teeth
- Change in bite or tooth alignment
The Complexity of Oral Microbiota
Diverse Microbial Environment
The mouth is home to a complex community of microorganisms, known as the oral microbiota. This community includes bacteria, viruses, fungi, and protozoa. There are over 700 different bacterial species that can inhabit the oral cavity. This diversity makes it challenging to pinpoint specific pathogens responsible for periodontal disease.
Biofilm Formation
Bacteria in the mouth form biofilms, which are structured communities of microorganisms attached to surfaces, such as teeth and gums. These biofilms protect the bacteria from the host’s immune system and antibiotics. The biofilm structure makes it difficult to isolate and identify individual pathogens.
Symbiotic Relationships
In the oral microbiota, some bacteria coexist peacefully with the host, while others can cause disease under certain conditions. This symbiotic relationship complicates the identification of pathogens because not all bacteria present in periodontal disease are harmful. Some may even play a protective role.
Limitations of Traditional Culturing Methods
Challenges of Culturing Oral Bacteria
Traditional methods of identifying bacteria involve culturing samples in a laboratory. However, many oral bacteria are difficult to culture. Some bacteria require specific growth conditions that are not easily replicated in the lab. As a result, many pathogens may go undetected using standard culturing methods.
Viable but Non-Culturable (VBNC) State
Some bacteria can enter a viable but non-culturable (VBNC) state, meaning they are alive but cannot be cultured using standard techniques. This state can occur due to environmental stress or nutrient deprivation. As a result, these bacteria may be present in periodontal disease but remain undetected.
The Role of Molecular Techniques
Advancements in Molecular Biology
Molecular techniques, such as polymerase chain reaction (PCR) and next-generation sequencing (NGS), have advanced the identification of oral pathogens. These techniques allow researchers to detect bacterial DNA directly from samples, bypassing the need for culturing. However, these methods also have limitations.
Detection of Non-Specific DNA
Molecular techniques can detect a wide range of bacterial DNA, but they do not differentiate between live and dead bacteria. This means that the presence of bacterial DNA does not necessarily indicate an active infection. The challenge lies in identifying which bacteria are actively contributing to periodontal disease.
Complexity of the Microbiome
The oral microbiome is highly complex, with many bacteria interacting in various ways. Identifying specific pathogens requires understanding these interactions. Some bacteria may enhance the pathogenicity of others, making it difficult to determine which bacteria are the primary culprits in periodontal disease.
Host Factors and Their Influence
Immune Response Variability
The host’s immune response plays a crucial role in the development of periodontal disease. Individual differences in immune response can influence the types of bacteria that thrive in the oral cavity. Factors such as genetics, age, and overall health can affect how the body reacts to oral bacteria, complicating the identification of specific pathogens.
Systemic Health Conditions
Certain systemic health conditions, such as diabetes and cardiovascular disease, can influence the oral microbiome and the host’s immune response. These conditions can create an environment that favors the growth of specific bacteria, making it challenging to identify the primary pathogens responsible for periodontal disease.
Environmental Factors
Oral Hygiene Practices
Oral hygiene practices significantly impact the composition of the oral microbiota. Poor oral hygiene can lead to an overgrowth of harmful bacteria, while good oral hygiene can help maintain a balanced microbiome. However, the variability in individual oral hygiene practices makes it difficult to establish a direct link between specific pathogens and periodontal disease.
Diet and Lifestyle
Diet and lifestyle factors, such as smoking and nutrition, can also influence the oral microbiome. For instance, a diet high in sugar can promote the growth of harmful bacteria. However, the interplay between diet, lifestyle, and specific pathogens is complex and not fully understood.
Implications of Difficulty in Identifying Pathogens
Challenges in Treatment
The difficulty in identifying specific pathogens associated with periodontal disease poses challenges for treatment. If the underlying causes are not well understood, it may be challenging to develop targeted therapies. Current treatments often focus on general plaque removal and improving oral hygiene rather than targeting specific pathogens.
Need for Personalized Medicine
The complexity of periodontal disease highlights the need for personalized medicine approaches. Understanding the unique microbial composition of an individual’s oral cavity could lead to more effective treatments tailored to their specific needs. However, this requires better identification of pathogens and their roles in disease progression.
Future Directions in Research
Improved Diagnostic Techniques
Future research should focus on developing improved diagnostic techniques that can accurately identify the pathogens involved in periodontal disease. This may involve refining molecular methods to differentiate between live and dead bacteria and understanding their interactions within the oral microbiome.
Longitudinal Studies
Longitudinal studies that track changes in the oral microbiome over time could provide insights into how specific bacteria contribute to the development of periodontal disease. By understanding the dynamics of the microbiome, researchers may be better equipped to identify pathogens and their roles in disease progression.
Collaboration Between Disciplines
Collaboration between dental professionals, microbiologists, and immunologists can enhance our understanding of periodontal disease. By combining expertise from different fields, researchers can develop a more comprehensive picture of the pathogens involved and their interactions with the host.
Conclusion
Identifying the pathogens responsible for periodontal disease is a complex challenge due to the diverse oral microbiota, limitations of traditional culturing methods, and the influence of host and environmental factors. While advancements in molecular techniques have improved our ability to detect oral bacteria, the intricacies of the microbiome and the interplay between different species complicate the identification of specific pathogens.
Addressing these challenges is crucial for developing effective treatments for periodontal disease. As research continues to evolve, a better understanding of the pathogens involved may lead to more targeted therapies and improved outcomes for individuals suffering from this common dental condition. By focusing on personalized approaches and enhancing diagnostic techniques, we can move closer to unraveling the complexities of periodontal disease and its pathogens.
Related topics: