Tooth decay is a widespread dental problem that affects individuals of all ages. While poor oral hygiene and high sugar intake are well-known contributors to tooth decay, certain diseases can also play a significant role in its development. In this article, we will explore various diseases that can lead to tooth decay, their mechanisms, and how they impact oral health.
Understanding Tooth Decay
1. What Is Tooth Decay?
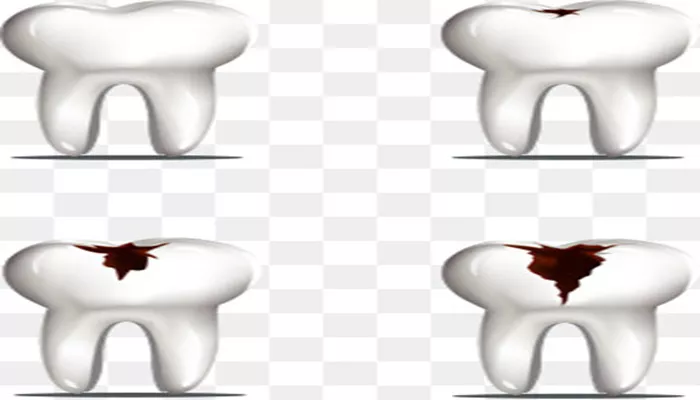
Tooth decay, also known as dental caries, is the process of demineralization of the tooth structure. It occurs when acids produced by bacteria in the mouth erode the enamel, the hard outer layer of the teeth. If left untreated, tooth decay can lead to cavities, pain, and even tooth loss.
2. How Does Tooth Decay Happen?
Tooth decay develops in several stages:
Plaque Formation: Bacteria in the mouth form a sticky film called plaque. This film develops when sugars from food and drinks interact with bacteria.
Acid Production: When you consume sugary or starchy foods, bacteria in plaque metabolize these sugars and produce acids.
Enamel Erosion: The acids attack the enamel, leading to its demineralization. Over time, this can create cavities.
Cavity Formation: If the decay process continues, it can lead to the formation of cavities, which are holes in the teeth.
Diseases That Cause Tooth Decay
1. Diabetes
Overview
Diabetes is a chronic condition that affects how your body processes blood sugar (glucose). Both type 1 and type 2 diabetes can increase the risk of tooth decay.
Mechanisms
Dry Mouth: Diabetes can lead to reduced saliva production, resulting in dry mouth. Saliva is essential for neutralizing acids and washing away food particles and bacteria.
High Blood Sugar: Elevated blood sugar levels can promote bacterial growth in the mouth, increasing the risk of plaque formation and tooth decay.
2. Sjögren’s Syndrome
Overview
Sjögren’s syndrome is an autoimmune disorder that primarily affects the glands that produce moisture in the body, including saliva and tears.
Mechanisms
Dry Mouth (Xerostomia): A significant symptom of Sjögren’s syndrome is dry mouth. Reduced saliva flow increases the risk of tooth decay because saliva helps neutralize acids and remineralize teeth.
Bacterial Growth: The lack of saliva creates an environment that allows harmful bacteria to thrive, leading to increased plaque and decay.
3. Gastroesophageal Reflux Disease (GERD)
Overview
Gastroesophageal reflux disease (GERD) is a digestive disorder where stomach acid flows back into the esophagus. This condition can have adverse effects on oral health.
Mechanisms
Acid Erosion: Repeated exposure to stomach acid can erode tooth enamel, making teeth more susceptible to decay.
Increased Sensitivity: Enamel erosion can lead to increased tooth sensitivity, which may discourage individuals from maintaining good oral hygiene.
4. Eating Disorders
Overview
Eating disorders, such as anorexia nervosa and bulimia nervosa, can significantly impact oral health and increase the risk of tooth decay.
Mechanisms
Nutritional Deficiencies: Individuals with eating disorders often have poor nutrition, leading to deficiencies in essential vitamins and minerals that support oral health.
Acid Exposure: Bulimia involves episodes of vomiting, which exposes teeth to stomach acid. This acid can erode enamel and lead to tooth decay.
5. Celiac Disease
Overview
Celiac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. This condition can also affect oral health.
Mechanisms
Nutritional Deficiencies: Celiac disease can lead to malabsorption of nutrients, resulting in deficiencies that can weaken teeth and gums.
Increased Risk of Cavities: The malabsorption of calcium and vitamin D can lead to weaker enamel, increasing the risk of tooth decay.
6. HIV/AIDS
Overview
HIV (Human Immunodeficiency Virus) and AIDS (Acquired Immunodeficiency Syndrome) can have significant effects on oral health.
Mechanisms
Weakened Immune System: Individuals with HIV/AIDS have compromised immune systems, making them more susceptible to infections, including oral infections.
Oral Candidiasis: This fungal infection can lead to dry mouth and other oral health issues, increasing the risk of tooth decay.
7. Hypertension
Overview
Hypertension, or high blood pressure, can also impact oral health, particularly when associated with certain medications.
Mechanisms
Medication Side Effects: Some antihypertensive medications can cause dry mouth as a side effect. Reduced saliva flow increases the risk of tooth decay.
Increased Plaque Buildup: A dry mouth environment can lead to increased plaque buildup, promoting decay.
The Impact of Medications on Tooth Decay
1. Antidepressants
Overview
Certain antidepressants can lead to dry mouth, increasing the risk of tooth decay.
Mechanisms
Reduced Saliva Production: Antidepressants can decrease saliva flow, creating an environment conducive to bacterial growth and tooth decay.
2. Antihistamines
Overview
Antihistamines, commonly used for allergies, can also cause dry mouth as a side effect.
Mechanisms
Dry Mouth: Like other medications that reduce saliva production, antihistamines can increase the risk of tooth decay by creating a dry oral environment.
Preventive Measures Against Tooth Decay
1. Maintain Good Oral Hygiene
Brush and Floss: Brush your teeth at least twice a day and floss daily to remove plaque and food particles.
Use Fluoride Products: Fluoride toothpaste and mouth rinses can help strengthen enamel and reduce the risk of decay.
2. Stay Hydrated
Drink Water: Staying hydrated can help maintain saliva production, which is essential for oral health.
Use Saliva Substitutes: For individuals with dry mouth, saliva substitutes can help keep the mouth moist.
3. Regular Dental Check-Ups
Professional Cleanings: Regular visits to the dentist for cleanings can help remove plaque and tartar buildup.
Early Detection: Dentists can identify early signs of tooth decay and provide treatment before it progresses.
4. Healthy Diet
Limit Sugary Foods: Reduce the intake of sugary and acidic foods that can promote tooth decay.
Eat Nutrient-Rich Foods: A balanced diet rich in vitamins and minerals supports overall health and oral health.
5. Address Underlying Health Issues
Manage Chronic Conditions: Proper management of chronic diseases like diabetes and GERD can help reduce the risk of tooth decay.
Consult Healthcare Providers: Work with healthcare providers to manage medications that may affect oral health.
Conclusion
Tooth decay is a multifaceted issue influenced by various factors, including certain diseases and medications. Conditions such as diabetes, Sjögren’s syndrome, GERD, eating disorders, and others can significantly increase the risk of tooth decay. Understanding these connections is essential for effective prevention and treatment.
By maintaining good oral hygiene, staying hydrated, eating a balanced diet, and managing underlying health conditions, individuals can reduce their risk of tooth decay. Regular dental check-ups are also crucial for early detection and intervention. If you have any concerns about your oral health or the impact of a specific disease on your teeth, consult with your dentist or healthcare provider for personalized guidance. Taking proactive steps can help protect your teeth and maintain a healthy smile.
Related topics: