Periodontal disease, commonly known as gum disease, is an inflammatory condition that affects the tissues surrounding the teeth. It starts with gingivitis and can progress to periodontitis if not treated. While periodontal disease primarily affects oral health, research has shown that it is also linked to several systemic diseases. Understanding these connections is essential for comprehensive patient care. In this article, we will explore the systemic diseases related to periodontal disease, how they are interconnected, and the implications for overall health.
What is Periodontal Disease?
Definition of Periodontal Disease
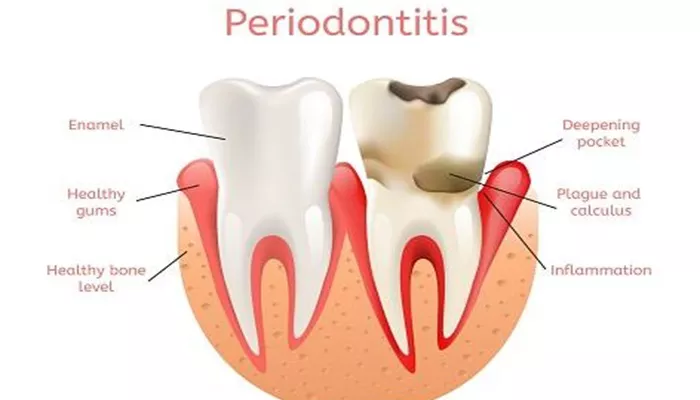
Periodontal disease is an infection of the gums and supporting structures of the teeth. It is caused by the accumulation of plaque, a sticky film of bacteria that forms on the teeth. If plaque is not removed through regular brushing and flossing, it can harden into tartar, leading to inflammation and infection of the gums.
Stages of Periodontal Disease
Gingivitis: The earliest stage, characterized by swollen, red, and bleeding gums. Gingivitis is often reversible with proper oral hygiene.
Early Periodontitis: In this stage, inflammation extends deeper, causing mild bone loss and the formation of pockets around the teeth.
Moderate Periodontitis: More significant bone loss occurs, and the pockets deepen, making it harder to maintain oral hygiene.
Advanced Periodontitis: Severe bone loss and deep pockets can lead to tooth mobility and potential tooth loss.
The Connection Between Periodontal Disease and Systemic Diseases
How Periodontal Disease Affects Overall Health
Research has shown that periodontal disease can have systemic effects beyond the mouth. The inflammation and bacteria associated with periodontal disease can enter the bloodstream, potentially affecting various organs and systems in the body. This connection explains why individuals with periodontal disease may be at greater risk for certain systemic diseases.
Systemic Diseases Linked to Periodontal Disease
1. Cardiovascular Disease
Cardiovascular disease is one of the most well-documented systemic diseases associated with periodontal disease. Studies have shown that individuals with periodontal disease are at a higher risk for heart disease, stroke, and other cardiovascular conditions. The proposed mechanisms include:
Inflammation: Chronic inflammation from periodontal disease can contribute to the development of atherosclerosis, a condition characterized by the buildup of plaque in the arteries.
Bacterial Invasion: Bacteria from periodontal infections can enter the bloodstream and contribute to the formation of blood clots, leading to heart attacks or strokes.
2. Diabetes
Diabetes and periodontal disease have a bidirectional relationship. People with diabetes are more susceptible to gum disease due to impaired immune response and increased inflammation. Conversely, periodontal disease can make it more challenging to control blood sugar levels. The connections include:
Inflammatory Response: Periodontal disease can lead to increased insulin resistance, making it harder for individuals with diabetes to manage their blood sugar.
Infection Risk: Diabetic individuals are more prone to infections, including periodontal infections, due to their compromised immune system.
3. Respiratory Diseases
There is a significant link between periodontal disease and respiratory diseases, including pneumonia and chronic obstructive pulmonary disease (COPD). The mechanisms behind this connection include:
Aspiration of Bacteria: Bacteria from periodontal infections can be aspirated into the lungs, leading to respiratory infections.
Inflammation: Chronic inflammation in the mouth can exacerbate existing respiratory conditions and increase the risk of lung infections.
4. Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune condition characterized by joint inflammation. Research suggests a connection between periodontal disease and RA. The potential links include:
Shared Inflammatory Pathways: Both conditions involve chronic inflammation, and the inflammatory mediators in periodontal disease may contribute to joint inflammation.
Bacterial Influence: Certain bacteria associated with periodontal disease may trigger immune responses that worsen rheumatoid arthritis.
5. Alzheimer’s Disease
Recent studies have suggested a possible link between periodontal disease and Alzheimer’s disease. The connections may involve:
Inflammation: Chronic inflammation from periodontal disease may contribute to neuroinflammation, a factor in the progression of Alzheimer’s disease.
Bacterial Presence: Some studies have found bacteria associated with periodontal disease in the brains of Alzheimer’s patients, suggesting a potential role in cognitive decline.
6. Pregnancy Complications
Pregnant women with periodontal disease may face increased risks of complications, including:
Preterm Birth: Research indicates that periodontal disease may be linked to preterm labor and low birth weight.
Gestational Diabetes: There is evidence that periodontal disease can increase the risk of developing gestational diabetes during pregnancy.
7. Kidney Disease
Chronic kidney disease (CKD) has also been associated with periodontal disease. The potential connections include:
Inflammation and Infection: Periodontal disease can exacerbate systemic inflammation, which may worsen kidney function.
Bacterial Translocation: Bacteria from periodontal infections may enter the bloodstream and affect kidney health.
Mechanisms of Interaction
Inflammation
Chronic inflammation is a common factor linking periodontal disease with systemic diseases. The inflammatory mediators released during periodontal infections can affect various body systems, leading to increased risks for conditions such as cardiovascular disease and diabetes.
Bacterial Spread
Periodontal pathogens can enter the bloodstream through inflamed gum tissues. Once in circulation, these bacteria can affect distant sites, contributing to infections and inflammation in other organs.
Immune Response
The immune response to periodontal disease can alter systemic health. A compromised immune system can lead to increased susceptibility to infections, including those in other parts of the body.
Prevention and Management
1. Good Oral Hygiene
Maintaining good oral hygiene is crucial for preventing periodontal disease and its potential systemic effects. This includes:
- Brushing teeth at least twice a day with fluoride toothpaste
- Flossing daily to remove plaque between teeth
- Using an antibacterial mouthwash to reduce bacteria
2. Regular Dental Check-ups
Regular visits to the dentist for cleanings and check-ups are essential for early detection and management of periodontal disease. Dentists can provide professional cleanings to remove plaque and tartar, and they can monitor gum health.
3. Managing Systemic Health Conditions
Individuals with systemic diseases should work closely with their healthcare providers to manage their overall health.
Controlling conditions such as diabetes and cardiovascular disease can help reduce the risk of periodontal disease.
4. Healthy Lifestyle Choices
Adopting a healthy lifestyle can significantly impact oral and systemic health. Key components include:
Balanced Diet: Eating a diet rich in fruits, vegetables, whole grains, and lean proteins supports both oral and overall health.
Regular Exercise: Physical activity can help reduce inflammation and improve immune function.
Avoiding Tobacco: Quitting smoking and using tobacco products can improve gum health and reduce the risk of systemic diseases.
5. Stress Management
Managing stress is important for overall health. Stress can negatively impact immune function and oral health. Techniques such as meditation, yoga, and exercise can help reduce stress levels.
Conclusion
Periodontal disease is not just an oral health issue; it is linked to several systemic diseases, including cardiovascular disease, diabetes, respiratory diseases, rheumatoid arthritis, Alzheimer’s disease, pregnancy complications, and kidney disease. The connections between these conditions highlight the importance of maintaining good oral health for overall well-being.
By understanding the links between periodontal disease and systemic health, individuals can take proactive steps to prevent gum disease and its potential complications. Regular dental care, good oral hygiene practices, and a healthy lifestyle are essential for maintaining both oral and systemic health. If you have concerns about your gum health or its impact on your overall health, it is important to consult a dental professional for evaluation and guidance.
Related topics: