Periodontal disease, commonly known as gum disease, is an inflammatory condition that affects the tissues surrounding the teeth. It begins with gingivitis, which can progress to periodontitis if not treated properly. While good oral hygiene and professional dental care are essential for managing periodontal disease, antibiotics can also play a crucial role in treatment.
This article will explore the types of antibiotics used to treat periodontal disease, how they work, and their effectiveness in managing this condition.
What is Periodontal Disease?
Definition of Periodontal Disease
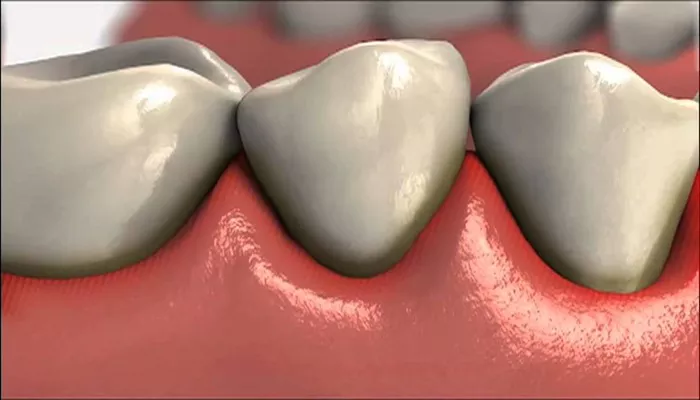
Periodontal disease is an infection of the gums and supporting structures of the teeth. It is caused primarily by the accumulation of plaque, a sticky film of bacteria that forms on the teeth. If plaque is not removed through regular brushing and flossing, it can harden into tartar, leading to inflammation and infection of the gums.
Stages of Periodontal Disease
Gingivitis: The earliest stage, characterized by swollen, red, and bleeding gums. Gingivitis is often reversible with proper oral hygiene.
Early Periodontitis: In this stage, inflammation extends deeper, causing mild bone loss and the formation of pockets around the teeth.
Moderate Periodontitis: More significant bone loss occurs, and the pockets deepen, making it harder to maintain oral hygiene.
Advanced Periodontitis: Severe bone loss and deep pockets can lead to tooth mobility and potential tooth loss.
The Role of Antibiotics in Treating Periodontal Disease
Why Use Antibiotics?
Antibiotics are used in conjunction with other treatments for periodontal disease. They help reduce the bacterial load in the mouth, control infection, and promote healing of the gum tissues. Antibiotics can be particularly beneficial in cases of:
Severe Periodontitis: When the infection is extensive and not responding to standard treatments.
Aggressive Periodontitis: A more severe form of gum disease that can occur in younger individuals.
Recurrent Periodontitis: When the disease returns after treatment.
How Antibiotics Work
Antibiotics work by targeting and killing bacteria or inhibiting their growth. In the case of periodontal disease, they help reduce the number of harmful bacteria in the mouth, allowing the immune system to regain control over the infection.
Common Antibiotics Used to Treat Periodontal Disease
Several antibiotics are commonly prescribed for treating periodontal disease. Here are some of the most effective ones:
1. Amoxicillin
Description: Amoxicillin is a broad-spectrum penicillin antibiotic. It is effective against a wide variety of bacteria, including those commonly found in periodontal infections.
Usage: Amoxicillin is often prescribed in combination with other antibiotics or treatments for periodontal disease. It is typically taken orally in pill form.
Dosage: The usual dosage for treating periodontal disease is 500 mg three times a day for 7 to 14 days, depending on the severity of the infection.
Effectiveness: Amoxicillin has been shown to reduce pocket depth and improve clinical attachment levels in patients with periodontitis.
2. Metronidazole
Description: Metronidazole is an antibiotic that is particularly effective against anaerobic bacteria, which thrive in low-oxygen environments like periodontal pockets.
Usage: Metronidazole can be used alone or in combination with amoxicillin for enhanced effectiveness. It can be taken orally or applied topically in gel form.
Dosage: For oral treatment, the typical dosage is 250 mg to 500 mg three times a day for 7 to 10 days.
Effectiveness: Metronidazole has been shown to significantly reduce inflammation and bacterial load in patients with periodontal disease.
3. Doxycycline
Description: Doxycycline is a tetracycline antibiotic that has both antibacterial and anti-inflammatory properties. It is effective against a range of bacteria associated with periodontal disease.
Usage: Doxycycline can be used as an adjunct to scaling and root planing (SRP) procedures. It can be taken orally or used in a controlled-release form placed directly in periodontal pockets.
Dosage: The typical oral dosage is 100 mg once daily for 7 to 14 days. For the controlled-release form, it is usually placed in the pocket by a dental professional.
Effectiveness: Doxycycline has been shown to improve clinical outcomes in patients with chronic periodontitis by reducing pocket depth and improving attachment levels.
4. Clindamycin
Description: Clindamycin is an antibiotic that is effective against anaerobic bacteria and is often used in patients who are allergic to penicillin.
Usage: Clindamycin is typically prescribed for patients with severe periodontal disease or those who do not respond to other antibiotics.
Dosage: The usual dosage is 150 mg to 300 mg every 6 hours for 7 to 10 days.
Effectiveness: Clindamycin has been shown to be effective in reducing periodontal pathogens and improving clinical outcomes in patients with periodontitis.
5. Azithromycin
Description: Azithromycin is a macrolide antibiotic that has a broad spectrum of activity against various bacteria, including those associated with periodontal disease.
Usage: Azithromycin is often used for patients with aggressive periodontitis or those who cannot tolerate other antibiotics.
Dosage: The typical dosage is 500 mg on the first day, followed by 250 mg once daily for the next 4 days.
Effectiveness: Azithromycin has been shown to improve clinical parameters in patients with periodontal disease and has a long half-life, allowing for shorter treatment courses.
Local Antibiotic Delivery Systems
In addition to systemic antibiotics taken orally, there are also local delivery systems that can be used to treat periodontal disease. These systems deliver antibiotics directly to the site of infection, providing concentrated treatment while minimizing systemic side effects.
1. Minocycline Microspheres
Description: Minocycline microspheres are small beads that contain the antibiotic minocycline. They are placed directly into periodontal pockets after scaling and root planing.
Effectiveness: Studies have shown that minocycline microspheres can reduce pocket depth and improve clinical attachment levels in patients with periodontitis.
2. Doxycycline Gel
Description: Doxycycline gel is a controlled-release formulation that is applied directly to periodontal pockets.
Effectiveness: The gel provides sustained release of doxycycline, allowing for prolonged antibacterial action at the site of infection.
3. Chlorhexidine Chip
Description: Chlorhexidine is an antiseptic that can be placed in periodontal pockets. It helps reduce bacteria and inflammation.
Effectiveness: Chlorhexidine chips have been shown to be effective in reducing pocket depth and improving periodontal health when used in conjunction with scaling and root planing.
Considerations and Side Effects
Potential Side Effects of Antibiotics
While antibiotics can be effective in treating periodontal disease, they may also have side effects. Common side effects include:
Gastrointestinal Issues: Nausea, vomiting, diarrhea, and abdominal pain are common side effects of many antibiotics.
Allergic Reactions: Some individuals may experience allergic reactions, ranging from mild rashes to severe anaphylaxis.
Antibiotic Resistance: Overuse or inappropriate use of antibiotics can lead to antibiotic resistance, making future infections harder to treat.
Importance of Professional Guidance
It is essential to use antibiotics under the guidance of a dental professional. A dentist can determine the appropriate antibiotic, dosage, and duration of treatment based on the severity of periodontal disease and the patient’s overall health.
Conclusion
Antibiotics can play a significant role in the treatment of periodontal disease, especially in cases of severe or aggressive forms of the condition. Common antibiotics used include amoxicillin, metronidazole, doxycycline, clindamycin, and azithromycin. Local delivery systems, such as minocycline microspheres and doxycycline gel, provide targeted treatment directly to the site of infection.
While antibiotics can be effective in managing periodontal disease, they should be used judiciously and under the supervision of a dental professional. Good oral hygiene practices, regular dental check-ups, and a healthy lifestyle are essential for preventing and managing periodontal disease. If you have concerns about your gum health or the need for antibiotic treatment, consult your dentist for personalized advice and care.
Related topics: